Translate this page into:
Clinical and Sociodemographic Characteristics Associated with Emergency Peripartum Hysterectomy due to Puerperal Sepsis in Malawi
* Corresponding author email: Amber Olson, ato8@case.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
In Malawi, emergency peripartum hysterectomy continues to be routine for the management of puerperal sepsis. While the hysterectomy may be life-saving for the mother, it carries with it life-altering permanent sterility. The surgeon is left with a difficult dilemma: remove the infection source (uterus) to preserve the life of the patient at the cost of her fertility, or preserve the uterus and fertility but risk worsening infection and possible death for the patient. The objective of this study was to (1) identify characteristics associated with mortality post-laparotomy due to puerperal sepsis and (2) identify characteristics associated with emergency peripartum hysterectomy in the management of puerperal sepsis.
Methods:
In this retrospective chart review, we obtained medical records of patients who underwent laparotomy secondary to puerperal sepsis at a tertiary hospital in Lilongwe, Malawi. Data collected included demographic information and clinical findings. These data were compared between women with and without adverse outcomes. Chi-squared tests were used to determine if there were significant relationships between variables and outcomes.
Results:
Fifty-eight patient records met inclusion criteria. The following characteristics were significantly associated with mortality: age greater than 30, multiparity, vaginal delivery, and intensive care unit admission. Cesarean delivery and an intraoperative finding of necrosis were significantly associated with hysterectomy.
Conclusion and Global Health Implications:
Emergency peripartum hysterectomy in the setting of puerperal sepsis is a significant source of maternal morbidity and mortality. To prevent emergency peripartum hysterectomy, it is important to have prompt recognition and treatment of puerperal sepsis, to have access to adequate antibiotics, and to have standards to guide the role of hysterectomy as the definitive and necessary treatment for puerperal sepsis.
Keywords
Cesarean Delivery
Emergency Peripartum Hysterectomy
Hysterectomy
Low-Resource Settings
Malawi
Maternal Morbidity
Maternal Mortality
Puerperal Sepsis
1. Introduction
1.1. Background of the Study
Emergency peripartum hysterectomy, defined as an emergency hysterectomy within 6 weeks postpartum, is used as a last resort treatment for life-threatening obstetric emergencies, including puerperal sepsis.1 The World Health Organization (WHO) defines puerperal sepsis as an infection that occurs between labor and 42 days postpartum with a fever and at least one of the following symptoms: pelvic pain, abnormal vaginal discharge, or delay in uterine involution.2 According to the WHO systematic analysis of maternal death between 2003 to 2009, puerperal sepsis accounted for 10.3% (134,000) of maternal deaths in sub-Saharan Africa – a percentage over twice as high as that of high resource countries (690, 4.7%).3
At the Ethel Mutharika maternity ward of Kamuzu Central Hospital, a 1,000-bed tertiary teaching hospital in the capital city of Lilongwe, Malawi, emergency peripartum hysterectomy continues to be routine for the management of severe puerperal sepsis. Hysterectomy is the definitive treatment for puerperal sepsis and may save a woman’s life, but also leads to permanent sterility and carries a risk of emotional damage, organ damage, and death. The fatality rate of emergency peripartum hysterectomy is the highest in low-resource settings.4 In its criteria for assessing maternal health quality of care, the WHO includes the performance of emergency peripartum hysterectomy secondary to infection as a “maternal near-miss” – an event in which a woman “nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of termination of pregnancy.”3,5
While the mortality associated with puerperal sepsis in sub-Saharan Africa is significant and exceeds that in high resource settings, we lack an accurate estimate of its true incidence and impact.6 Estimates of the incidence of puerperal sepsis range from 0.1% to 10%.7 Case fatality rates range between 30% and 50% in low and middle-income countries.8 The wide range of statistics reflect poor documentation and record-keeping, as well as limited and inadequate microbiological specimens.
The development of puerperal sepsis is a common indication for emergency peripartum hysterectomy in low-resource settings. Recent studies in South Africa found that puerperal sepsis was a primary indication for emergency peripartum hysterectomy in up to 46% of cases.4,9,10 A standard protocol guiding emergency peripartum hysterectomy secondary to puerperal sepsis remains unclear and there is a scarcity of recent literature regarding clinical course and outcomes in settings with limited access to antibiotics. As a result, the incidence of emergency peripartum hysterectomy is greatly influenced by clinical impression and factors such as delayed recognition of puerperal sepsis, availability of adequate antibiotics, and delays in transfer to specialist care at the tertiary center.4,11 The surgeon is left with a difficult dilemma: remove the infection source (uterus) to preserve the life of the patient at the cost of her fertility, or preserve the uterus and fertility but risk worsening infection and possible death for the patient.
1.2. Objectives of the Study
To our knowledge, no studies exist that specifically examined emergency peripartum hysterectomy secondary to puerperal sepsis in Malawi, and few studies have investigated the problem in greater sub-Saharan Africa. A recent study in South Africa found that emergency peripartum hysterectomy due to puerperal sepsis was higher than previously reported and had worse outcomes than hemorrhage-related emergency peripartum hysterectomy.4 A study investigating maternal near-miss in Rwanda observed the lack of a standard protocol for managing puerperal sepsis with emergency peripartum hysterectomy.11 The primary objective of this study, therefore, was to identify demographic and clinical characteristics associated with mortality for women undergoing laparotomy due to puerperal sepsis in Malawi. The secondary objective was to identify characteristics associated with emergency peripartum hysterectomy in the management of puerperal sepsis.
1.3. Specific Aims and Hypothesis
We hope to use significant characteristics (1) to improve patient care, (2) to determine if and when emergency peripartum hysterectomy is necessary for the management of puerperal sepsis, and (3) to avoid adverse events in the management of puerperal sepsis in Malawi and other low resource settings.
2. Methods
In this descriptive retrospective chart review, we identified patients who underwent postpartum exploratory laparotomy [0-42 days postpartum] secondary to puerperal sepsis, peritonitis, and/or endometritis at the Ethel Mutharika maternity ward of Kamuzu Central Hospital, a tertiary teaching hospital in Lilongwe, Malawi between January 2017 and December 2017. We reviewed the hospital’s operative log to identify patients who met the inclusion criteria: women aged 12-49 who underwent postpartum laparotomy for a pre-operative clinical diagnosis of puerperal sepsis, peritonitis, and/or endometritis. We then obtained medical records of all identified patients who met the inclusion criteria to record detailed information regarding the operation and clinical course of these patients (Figure 1). Data collection sheets were de-identified and entered into a secure, encrypted database.
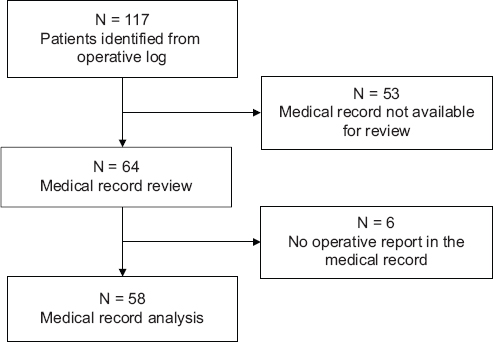
- Inclusion Flow Diagram
2.1. Study Variables
The independent variables included the adverse outcomes of mortality and emergency peripartum hysterectomy. The outcome variables included demographic information, clinical history at admission, physical exam findings, operative details, and hospital course. The data were compared between women with adverse outcomes of death and emergency peripartum hysterectomy and those with no adverse outcomes. Outcome variables included age, parity, referral source, delivery location, delivery mode, the outcome of the neonate, vital signs at admission, clinical diagnosis, operative findings, intensive care unit (ICU) admission, antibiotics, and length of hospital stay.
2.2. Statistical Analysis
Baseline and demographic characteristics were summarized using descriptive statistics. Chi-squared tests were used to determine if there were significant relationships between variables and outcomes (with a p-value of <0.05 set for statistical significance). All data analyses were conducted using R (version 3·5·1), RStudio (version 1·1·423).12, 13
2.3. Ethical Approval
Study approval was granted by the National Health Science Review Committee of Malawi and the Baylor College of Medicine Institutional Review Board. Informed consent was waived due to the retrospective nature of the study. All data were de-identified at the time of chart review.
3. Results
3.1. Sociodemographic Characteristics
Fifty-eight patient records were identified that met inclusion criteria and included detailed operative reports for review. We compared demographic, admission, and clinical variables with respect to mortality outcomes for women undergoing laparotomy secondary to puerperal sepsis (Table 1). In our cohort, 46 (79%) patients survived, and 12 (21%) patients died. The case fatality rate was 20.7%.
| Death (n=12) | % | Survival (n=46) | % | p-value | |
|---|---|---|---|---|---|
| Age | 0.0263 | ||||
| <=20 years | 3 | 25.0% | 21 | 45.7% | |
| 21-30 years | 5 | 41.7% | 23 | 50.0% | |
| >= 31 years | 4 | 33.3% | 2 | 4.3% | |
| Primiparous | 0.0037 | ||||
| Yes | 2 | 16.7% | 29 | 63.0% | |
| No | 10 | 83.3% | 15 | 32.6% | |
| Missing | 0 | 0.0% | 2 | 4.3% | |
| Status of Neonate | 0.0329 | ||||
| Live birth OR neonatal death | 4 | 33.3% | 30 | 65.2% | |
| Fresh/Macerated Stillbirth | 6 | 50.0% | 7 | 15.2% | |
| Missing | 2 | 16.7% | 9 | 19.6% | |
| Referral From | 0.744 | ||||
| District Hospital | 9 | 75.0% | 35 | 76.1% | |
| Health Center | 1 | 8.3% | 1 | 2.2% | |
| Other | 1 | 8.3% | 4 | 8.7% | |
| KCH | 1 | 8.3% | 3 | 6.5% | |
| Unknown | 0 | 0.0% | 3 | 6.5% | |
| Mode of Delivery | 0.0073 | ||||
| Vaginal Delivery | 5 | 41.7% | 5 | 10.9% | |
| Cesarean Delivery | 5 | 41.7% | 39 | 84.8% | |
| Unknown | 2 | 16.7% | 2 | 4.3% | |
| Delivery Location | 0.0071 | ||||
| Kamuzu Central Hospital | 0 | 0.0% | 9 | 19.6% | |
| District Hospital | 6 | 50.0% | 30 | 65.2% | |
| Health Center | 2 | 16.7% | 0 | 0.0% | |
| Private Hospital | 0 | 0.0% | 2 | 4.3% | |
| Home | 0 | 0.0% | 2 | 4.3% | |
| Unknown | 4 | 33.3% | 3 | 6.5% | |
| Previous Cesarean Delivery | 0.182 | ||||
| No | 8 | 66.7% | 37 | 80.4% | |
| Yes | 1 | 8.3% | 6 | 13.0% | |
| Missing | 3 | 25.0% | 3 | 6.5% | |
3.2. Factors Associated with Mortality
The following demographic and admission characteristics were significantly associated with mortality: maternal age 31 and older, multiparity, and vaginal delivery (Table 1). ICU admission was also significantly associated with mortality (Table 2).
| Death (n=12) | % | Survival (n=46) | % | p-value | |
|---|---|---|---|---|---|
| Length of Time from Delivery to Surgery (days) | 0.336 | ||||
| <=10 | 3 | 25.0% | 19 | 41.3% | |
| 11 to 20 | 6 | 50.0% | 21 | 45.7% | |
| 21 to 30 | 2 | 16.7% | 1 | 2.2% | |
| 31 to 40 | 1 | 8.3% | 4 | 8.7% | |
| Missing | 0 | 0.0% | 1 | 2.2% | |
| Indication for Surgery | 0.654 | ||||
| Peritonitis | 10 | 83.3% | 40 | 87.0% | |
| Burst abdomen | 2 | 16.7% | 3 | 6.5% | |
| Necrotic uterus | 0 | 0.0% | 2 | 4.3% | |
| Abscess | 0 | 0.0% | 1 | 2.2% | |
| Operation Performed | 0.979 | ||||
| Exploratory laparotomy | 3 | 25.0% | 15 | 32.6% | |
| Total abdominal hysterectomy | 5 | 41.7% | 18 | 39.1% | |
| Subtotal hysterectomy | 2 | 16.7% | 8 | 17.4% | |
| Hysterectomy+salpingectomy | 0 | 0.0% | 0 | 0.0% | |
| Hysterectomy+salpingo-oophorectomy | 1 | 8.3% | 3 | 6.5% | |
| Exploratory laparotomy+salpingo-oophorectomy | 1 | 8.3% | 2 | 4.3% | |
| Hysterectomy Performed | 0.945 | ||||
| No | 3 | 25.0% | 12 | 26.1% | |
| Yes | 9 | 75.0% | 34 | 73.9% | |
| Intraoperative Findings | 0.511 | ||||
| Necrotic uterus OR necrotic uterus+ovaries/tubes OR necrotic ovaries | 8 | 66.7% | 29 | 63.0% | |
| Bowel perforation/adhesions OR abscess OR hysterectomy dehiscence OR wound infection | 3 | 25.0% | 16 | 34.8% | |
| Missing | 1 | 8.3% | 1 | 2.2% | |
| EBL (mL) | 0.958 | ||||
| <500 | 5 | 10.9% | 8 | 17.4% | |
| 500-<1000 | 2 | 4.3% | 11 | 23.9% | |
| >=1000 | 0 | 0.0% | 3 | 6.5% | |
| Missing | 5 | 10.9% | 14 | 30.4% | |
| Antibiotics | 0.834 | ||||
| Ceftriaxone+metronidazole | 7 | 58.3% | 24 | 52.2% | |
| Ceftriaxone+metronidazole+gentamicin/meropenem/[piperacillin+tazobactam] | 5 | 41.7% | 21 | 45.7% | |
| Missing | 0 | 0.0% | 1 | 2.2% | |
| Re-laparotomy | 0.627 | ||||
| No | 9 | 75.0% | 34 | 73.9% | |
| Yes | 3 | 25.0% | 12 | 26.1% | |
| Intensive Care Admission | 0.0279 | ||||
| No | 8 | 66.7% | 43 | 93.5% | |
| Yes | 3 | 25.0% | 3 | 6.5% | |
| Missing | 1 | 8.3% | 0 | 0.0% | |
| Post-Operative Complications | 0.143 | ||||
| None | 4 | 33.3% | 6 | 13.0% | |
| Wound infection | 4 | 33.3% | 29 | 63.0% | |
| Wound infection+fascial dehiscence | 0 | 0.0% | 1 | 2.2% | |
| Wound infection+bladder injury | 0 | 0.0% | 2 | 4.3% | |
| Wound infection+bowel obstruction | 0 | 0.0% | 1 | 2.2% | |
| Renal failure | 2 | 16.7% | 1 | 2.2% | |
| Missing | 2 | 16.7% | 6 | 13.0% | |
| PPD at discharge or death | 0.07 | ||||
| <=10 | 3 | 25.0% | 0 | 0.0% | |
| 11 to 20 | 2 | 16.7% | 7 | 15.2% | |
| 21 to 30 | 3 | 25.0% | 14 | 30.4% | |
| 31 to 40 | 2 | 16.7% | 10 | 21.7% | |
| 41 to 50 | 1 | 8.3% | 7 | 15.2% | |
| > 50 | 1 | 8.3% | 8 | 17.4% | |
EBL=estimated blood loss PPD=postpartum day
3.3. Covariates for Emergency Peripartum Hysterectomy
We also identified characteristics associated with the risk of undergoing an emergency peripartum hysterectomy (Table 3). In our cohort, 43 (74%) patients underwent a hysterectomy, and 15 (26%) patients did not undergo a hysterectomy. Two variables were significantly associated with the risk of undergoing an emergency peripartum hysterectomy: 1) Cesarean as the mode of delivery and 2) an intraoperative finding of necrosis. Age, parity, the status of the neonate, delivery location, and intensive care admission were not significantly associated with the risk of undergoing an emergency peripartum hysterectomy (Table 3).
| No Hysterectomy (n=15) | % | Hysterectomy (n=43) | % | p-value | |
|---|---|---|---|---|---|
| Age | 0.916 | ||||
| <=20 years | 7 | 46.7% | 17 | 39.5% | |
| 21-30 years | 7 | 46.7% | 21 | 48.8% | |
| >= 31 years | 1 | 6.7% | 5 | 11.6% | |
| Primiparous | 0.563 | ||||
| Yes | 7 | 46.7% | 18 | 41.9% | |
| No | 7 | 46.7% | 25 | 58.1% | |
| Missing | 1 | 6.7% | 1 | 2.3% | |
| Mode of delivery | <0.0001 | ||||
| Spontaneous vaginal delivery | 8 | 53.3% | 2 | 4.7% | |
| Cesarean delivery | 6 | 40.0% | 38 | 88.4% | |
| Unknown | 1 | 6.7% | 3 | 7.0% | |
| Status of Neonate | 0.401 | ||||
| Live birth OR neonatal death | 11 | 73.3% | 23 | 53.5% | |
| Fresh/Macerated Stillbirth | 2 | 13.3% | 11 | 25.6% | |
| Missing | 2 | 13.3% | 9 | 20.9% | |
| Delivery Location | 0.0531 | ||||
| Kamuzu Central Hospital | 4 | 26.7% | 5 | 11.6% | |
| District Hospital | 6 | 40.0% | 30 | 69.8% | |
| Health Center | 1 | 6.7% | 1 | 2.3% | |
| Private Hospital | 0 | 0.0% | 2 | 4.7% | |
| Home | 2 | 13.3% | 0 | 0.0% | |
| Unknown | 2 | 13.3% | 5 | 11.6% | |
| Clinical Impression | 0.0024 | ||||
| Peritonitis OR peritonitis+Endometritis OR peritonitis+necrotic uterus OR endometritis | 14 | 93.3% | 37 | 86.0% | |
| Peritonitis+bowel obstruction OR other | 0 | 0.0% | 4 | 9.3% | |
| Missing | 1 | 6.7% | 2 | 4.7% | |
| Intraoperative Findings | 0.0044 | ||||
| Necrotic uterus OR necrotic uterus+ovaries/tubes OR necrotic ovaries | 4 | 26.7% | 33 | 76.7% | |
| Bowel perforations/adhesions OR abscess OR hysterotomy dehiscence OR wound infection | 10 | 66.7% | 9 | 20.9% | |
| Missing | 1 | 6.7% | 1 | 2.3% | |
| Intensive Care Admission | 0.712 | ||||
| No | 14 | 93.3% | 37 | 86.0% | |
| Yes | 1 | 6.7% | 5 | 11.6% | |
| Missing | 0 | 0.0% | 1 | 2.3% | |
4. Discussion
The primary objective of this study was to identify demographic and clinical characteristics associated with mortality for women undergoing laparotomy secondary to puerperal sepsis, peritonitis, and/or endometritis in Malawi. The secondary objective was to identify risk factors associated with emergency peripartum hysterectomy.
We found that maternal age greater than or equal to 31 was associated with an increased risk of mortality. Contrary to our findings, a retrospective study of patients at the University Teaching Hospital of Kigali in Rwanda found no difference between age groups in mortality rates due to laparotomy secondary to postpartum infection.11 Bauserman et al. found that after adjusting for various maternal risk factors, women delivered in the Democratic Republic of Congo, Guatemala, India, Kenya, Pakistan, and Zambia had a higher risk of mortality when maternal age was over 35 years old.14
We also found that multiparity was associated with an increased risk of mortality in women undergoing laparotomy, likely because the rate of obstetric complications, including postpartum hemorrhage, increases with parity.1 Our data is consistent with other studies: Bauserman et al. found an increased risk of maternal mortality when parity was greater than two.14 A study in Southwest Ethiopia found that the odds of maternal near-misses among multiparous women were 2.5 times that of nulliparous women.15
Cesarean mode of delivery was significantly associated with a risk of undergoing an emergency peripartum hysterectomy in our sample of women in Malawi. Seventy-six percent of our cohort delivered via cesarean.16 Similarly, the study in Rwanda found that 81% of patients who underwent laparotomy secondary to peripartum infection delivered via cesarean.11 Researchers at Jordan University Hospital also found emergency peripartum hysterectomy to be more common following cesarean compared to vaginal delivery.16 These results reflect the 20-fold increased risk of infection with cesarean compared to vaginal delivery.17 Of note, the rate of cesarean delivery in our cohort far exceeds the cesarean delivery rate in sub-Saharan Africa, which is just 5%, compared to 27.2% in high resource countries.18 This finding further underscores the greatly increased infection rate associated with cesarean compared to vaginal deliveries.
An intraoperative finding of necrosis was also significantly associated with the risk of undergoing hysterectomy in our cohort. Surgeons must use their clinical experience and subjective judgment during a laparotomy to determine if an emergency peripartum hysterectomy is necessary. The decision to perform a hysterectomy versus opt for fertility-sparing conservative management is complex, reflecting operative findings, the availability of antibiotics, and a woman’s clinical condition. The development of standard management guidelines for puerperal sepsis along with improved access to emergency obstetric care, laboratory studies, microbiology studies, and antibiotic access will help reduce emergency peripartum hysterectomy in low-resource settings.
Interestingly, vaginal delivery rather than cesarean delivery was significantly associated with mortality in our cohort. This finding contrasted with other studies which have found that cesarean delivery increases the rate of maternal mortality. The study in Rwanda found cesarean delivery to be significantly associated with maternal mortality.11 In addition, the African Surgical Outcomes study found that African women are at least 50 times more likely to die after cesarean delivery than their counterparts in high-income countries.19 The difference in our cohort may reflect delays in diagnosis of puerperal sepsis and a subsequent delay in surgical care for patients who had routine vaginal deliveries.
4.1. Strengths and Limitations of the study
The main strength of our study is that it is the first, to our knowledge, to examine risk factors of mortality and emergency peripartum hysterectomy secondary to puerperal sepsis in Malawi. The main limitations of this study were its retrospective design and lack of baseline data and statistics for the hospital, including cesarean delivery rate and puerperal sepsis rates. Many of the medical charts we reviewed had missing data on relevant variables. A majority of the patients in the cohort were delivered at outlying hospitals, and no delivery records were available to investigate the antepartum and delivery course; we could not ascertain when signs of puerperal infection might have first developed or what antibiotic treatment, if any, they had received prior to transfer. In addition, our cohort came from a tertiary teaching hospital in Lilongwe, Malawi, which may not be generalizable to all low-resource settings.
5. Conclusion and Global Health Implications
Emergency peripartum hysterectomy secondary to puerperal sepsis is a significant source of maternal morbidity and mortality in low-resource settings. Our study showed that cesarean delivery is significantly associated with emergency peripartum hysterectomy secondary to puerperal sepsis. To prevent unnecessary emergency peripartum hysterectomy in low-resource settings, it is important to prevent, recognize, and quickly treat puerperal sepsis, especially for patients undergoing cesarean delivery, which carries a much higher risk of infection compared to vaginal delivery. It is also important to develop standardized guidelines for the surgical management of puerperal sepsis and the appropriate use of emergency peripartum hysterectomy as a last-resort treatment. Finally, improved access to laboratory studies to inform clinical conditions, microbiology specimens to guide antibiotic treatment, and access to appropriate antibiotics for both prophylaxis and treatment will significantly reduce the morbidity and mortality associated with puerperal sepsis and reduce the use of emergency peripartum hysterectomy as its treatment. Future research should prospectively examine the relationships between cesarean delivery, puerperal sepsis, emergency peripartum hysterectomy, and maternal mortality in low-resource settings.
Acknowledgments:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflict of interest.
Financial Disclosure: The authors declare that they have no financial disclosures.
Funding/Support: Funding for this study was from the Baylor College of Medicine, Texas, United States.
Ethical Approval: Study approval was granted by the National Health Science Review Committee of Malawi and the Baylor College of Medicine Institutional Review Board.
Disclaimer: None.
References
- Prevalence, indications, risk indicators, and outcomes of emergency peripartum hysterectomy worldwide. Obstet Gynecol. 2016;128(6):1281-94. doi:10.1097/AOG.0000000000001736
- [Google Scholar]
- 1996. Maternal Health and Safe Motherhood Programme Division of Family Health, World Health Organization. https://apps.who.int/iris/handle/10665/63268
- Global causes of maternal death:a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323-33. doi:10.1016/S2214-109X(14)70227-X
- [Google Scholar]
- A district-wide population-based descriptive study of emergency peripartum hysterectomy in a middle-income country. Int J Gynaecol Obstet. 2019;146(1):103-9. doi:10.1002/ijgo.12837
- [Google Scholar]
- Maternal and early onset neonatal bacterial sepsis:burden and strategies for prevention in sub-Saharan Africa. Lancet Infect Dis. 2009;9(7):428-38. doi:10.1016/S1473-3099(09)70172-0
- [Google Scholar]
- Puerperal sepsis in low- and middle-income settings:past, present and future. In: Kehoe S, Neilson J, Norman J, eds. Maternal and Infant Deaths:Chasing Millennium Development Goals 4 and 5. Royal College of Obstetricians and Gynaecologists Study Group. Cambridge: Cambridge University Press; 2010. p. :131-148. doi:10.1017/CBO9781107784758.011
- [Google Scholar]
- Global Burden of Maternal Sepsis in the Year 2000. Evidence and Information for Policy (EIP), World Health Organization 2003
- [Google Scholar]
- Puerperal pyrexia:a review. Part I. Obstet Gynecol Surv. 2007;62(6):393-9. doi:10.1097/01.ogx.0000265998.40912.5e
- [Google Scholar]
- Sepsis:Primary indication for peripartum hysterectomies in a South African setting. S Afr J Obstet Gynaecol. 2016;22(2):52-6.
- [Google Scholar]
- Maternal near miss and mortality due to postpartum infection:a cross-sectional analysis from Rwanda. BMC Pregnancy Childbirth. 2016;16(1):177. doi:10.1186/s12884-016-0951-7
- [Google Scholar]
- R-Project. Published 2019 https://www.R-project.org/
- RStudio. Published 2020 http://www.rstudio.com
- Maternal mortality in six low and lower-middle income countries from 2010 to 2018:risk factors and trends. Reprod Health. 2020;17(3):173. doi:10.1186/s12978-020-00990-z
- [Google Scholar]
- Incidence-proportion of maternal near-misses and associated factors in Southwest Ethiopia:a prospective cross-sectional study. Int J Womens Health. 2020;12:1125-1134. doi:10.2147/IJWH.S283122
- [Google Scholar]
- Emergency peripartum hysterectomy at Jordan University hospital–a teaching hospital experience. Prz Menopauzalny. 2020;19(2):66-71. doi:10.5114/pm.2020.97840
- [Google Scholar]
- Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database of Syst Rev. 2014;2014(10):CD007482. doi:10.1002/14651858.CD007482.pub3
- [Google Scholar]
- Trends and projections of caesarean section rates:global and regional estimates. BMJ Glob Health. 2021;6(6):e005671. doi:10.1136/bmjgh-2021-00567
- [Google Scholar]
- Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study:a 7-day prospective observational cohort study. Lancet Glob Health. 2019;7(4):e513-22. doi:10.1016/S2214-109X(19)30036-1
- [Google Scholar]





