Translate this page into:
HIV Non-Occupational Post Exposure Prophylaxis in Nigeria: A Systematic Review of Research Evidence and Practice
*Corresponding author email: Ejessien@central.uh.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Although non-occupational Human Immunodeficiency Virus (HIV) post-exposure prophylaxis (nPEP) has been proven to be efficacious in preventing HIV, it remains an underutilized prevention strategy in Nigeria. We aimed to conduct an overview of research studies on nPEP and practice in Nigeria from 2002 to 2018 examining: sociodemographic characteristics of study sample, awareness, knowledge and prior use of nPEP, reasons for HIV nPEP, timeliness in presenting for PEP, antiretrovirals (ARVs) used for nPEP, side effects and adherence, monitoring and follow-up visits, adherence to guidelines and recommendations for nPEP by healthcare institutions and the strength of evidence of reviewed studies.
Methods:
An electronic search on PubMed, PubMed Central (PMC), cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Medline, Embase and Google Scholar for published studies on nPEP from January 2002 to December 2018. We conducted our search using different combinations of the keywords “HIV,” “non-occupational,” “nonoccupational,” “post-exposure,” “postexposure,” “prophylaxis” and “Nigeria.”
Results:
Five articles met the inclusion criteria for this study. About 25.4% of college students were aware of PEP.PEP awareness was significantly determined by the following factors ever tested for HIV, nude picture exchanges, sex without condom, and knowledge of partner’s HIV status. Across studies, exposed victims who presented for PEP were mostly females (64%-78%). Rape was the most frequently occurring reason for seeking nPEP (25.9%-64.1%). Although most patients presented for nPEP within 72 hours, follow up visits were generally low (0%-2%) across studies assessed, except for one study that reported a high follow up visit of 83.3%. Guidelines adherence by healthcare institutions could not be established due to lack of information on key variables.
Conclusion:
Our study highlights the paucity of research evidence on nPEP use in Nigeria, the societal and cultural contexts in which non-occupational exposures occur, healthcare providers’ roles and the public health and practice implications.
Keywords
HIV
post-exposure
prophylaxis
non-occupational
Prevention
Nigeria
1. Background and Introduction
Of the 37.9 million people living with the human immunodeficiency virus (HIV) globally, Africa alone accounts for about 25.7 million1 with Sub-Saharan Africa making up about 61% of the global burden of AIDS mortality in 2018.2 The 2018 Nigeria HIV/AIDS Indicator and Impact Survey shows that about 1.9 million Nigerians are currently living with HIV.3 With overall prevalence rate of 1.4% nationwide,4 Nigeria is among countries worst hit by HIV. In 2018, there were 130,000 persons newly infected with HIV in Nigeria and over 50,000 deaths due to AIDS,5,6 indicating that HIV/AIDS remains a serious public health threat to Nigeria. Furthermore, several studies have shown that HIV/AIDS in Nigeria has severe economic consequences on families and the country as a whole.7-10 Low risk perception, low condom use during high risk sex, multiple sexual partners, and poor access to quality HIV health and prevention services are among the main factors that continue to drive the spread of HIV in Nigeria.11 In addition, environmental factors such as improper disposal of hazardous waste, and some structural drivers such as poverty, gender inequality, human rights violations and stigma also increase the vulnerability of people to HIV in Nigeria.4
Although avoiding exposure to the virus remains the most effective method of preventing infection,12 studies have provided evidence for the efficacy of post-exposure prophylaxis (PEP), in preventing HIV infection within 72 hours of exposure,13-16 yet it remains an underutilized prevention strategy in Nigeria. HIV PEP refers to taking a 28-day course of antiretroviral (ARV) drugs within 72 hours of exposure to prevent HIV infection.12 When administered specifically following non-occupational exposure, it is referred to as non-occupational post-exposure prophylaxis (nPEP).12 In the context of this review, non-occupational exposure is defined as direct mucosal, percutaneous or intravenous contact to potentially infectious body fluids containing HIV, which occurs outside perinatal or occupational situations.17
One of the strategic goals of the Federal Ministry of Health in Nigeria is to significantly reduce the incidence of new HIV infections by enhancing access to HIV prevention, intervention and HIV prophylaxis by 90% in the general population.4 Although the National HIV and AIDS Strategic Framework (NASF), which serves as the blueprint for the fight against HIV/AIDS in Nigeria has prevention as one of its thematic areas,4,7 the framework does not mention the use of nPEP specifically as part of its strategy.4 However, the National Guideline for HIV Prevention, Treatment and Care by the Federal Ministry of Health, Nigeria, provides a detailed guideline on nPEP following sexual assault.18
Unlike occupational exposure,19-23 studies have shown that sexual assault accounts for most non-occupational exposure to HIV in sub-Saharan Africa.24,25 Among adults living with HIV in Nigeria, women accounted for an estimated 55.56%.26 This high figure may not be entirely uncorrelated with the fact that most victims of sexual assault are women.24 Although some studies have documented sexual assault in Nigeria,27-29 accurate statistics is lacking on the prevalence and type of services offered to victims.30 A study carried out in Lagos state, Nigeria, reported that 93.8% of sexual assault victims who presented at the hospital were females,31 corresponding to several other sexual assault studies in Nigeria28,32,33 and Sub-Saharan Africa.34,35 Sexual assault is often associated with physical trauma, genital trauma, multiple and unknown assailants, concurrent sexually transmitted diseases, psychological trauma and stigmatization,36,37 all which further increases the risk of HIV transmission.24 Exposed victims who are at high risk of HIV infection will be more likely to benefit from nPEP if they know where to receive nPEP services, present on time for it and are provided with quality care based on evidence-based medicine in line with the recommended guidelines.
As demonstrated by different studies, HIV infection is associated with significantly increased medical costs,9,38 hence, for every HIV infection averted by nPEP, significant cost savings can be gained. This is in line with a study conducted in the United States that reported a potential saving of $229,800 in lifetime medical cost for each unit of HIV infection prevented in the United States.39 A major barrier to accessing nPEP services is lack of knowledge on HIV prevention especially among young people between the ages of 15-24 who also happen to engage more in risky sexual behaviors and have low perception of HIV risk.40
One of the targets of the prevention strategy outlined in the National HIV and AIDS Strategic Framework is to ensure that 90% of the population including vulnerable and key groups access combination prevention services by 2020, and 95% by 2030 with the aspiration of ending the AIDS epidemic by 2030.4 Ensuring effective delivery of quality HIV prevention, treatment, care, support and adherence programs through strengthened health care system is one of the fundamental principles that guide the NASF.4 It is important therefore to assess the level of knowledge and use of nPEP services among important vulnerable groups and the quality of care provided for these individuals so as to inform interventions to achieve Nigeria’s HIV prevention goals. There is a dearth of literature on the level of knowledge of nPEP among non-health care workers and their pattern of use of nPEP services in Nigeria. Furthermore, no previous study has assessed the quality of nPEP care provided to individuals exposed to HIV with respect to how well institutions adhered to the standard of care recommended in the guideline by the Nigerian Federal Ministry of Health. A systematic review of literature on nPEP in sub-Saharan Africa also noted a paucity of research on nPEP in the region.24 This gap in knowledge represents a missed opportunity to support decision makers to make informed decision on nPEP, and thus, could potentially stall the achievement of Nigeria’s goal on HIV prevention and treatment.
We aimed to conduct an overview of research studies on nPEP and practice in Nigeria from 2002 to 2018 examining: (a) sociodemographic characteristics of study sample, (b) awareness, knowledge and prior use of PEP, (c) reasons for HIV nPEP, (d) timeliness in presenting for PEP, (e) ARVs used for nPEP, side effects and adherence, (f) monitoring and follow-up visits, (g) adherence to guidelines and recommendations for nPEP by healthcare institutions, and (h) the strength of evidence of reviewed studies. It attempts to highlight important areas to target for improvement of clinical practices in the area of nPEP service delivery. The findings of this review will be useful in identifying knowledge gaps and missed opportunities to strengthen the body of evidence in nPEP research and practice. This review will also be useful in supporting various nPEP stakeholders in making informed decision in HIV prevention strategies, policies and program designs in Nigeria.
2. Methods
2.1. Data Source and Literature Search
We conducted electronic searches on PubMed, PubMed Central (PMC), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Medline, Embase and Google Scholar for published studies from January 2002 to December 2018 using various combinations of the following keywords: “HIV”, “non-occupational”, “nonoccupational”, “post exposure”, “post-exposure”, “prophylaxis,” and “Nigeria”.
2.2. Study Selection
2.2.1. Inclusion/Exclusion criteria
Articles were included, if they were original research studies conducted in Nigeria, substantially included nPEP and were published in English language. Studies were also included, if they reported data on both PrEP, PEP and nPEP services but only data from nPEP were abstracted. Items were excluded if they were duplicates or irrelevant to nPEP. All conference abstracts, non-research and unpublished articles and newspaper articles were also excluded.
2.2.2. Selection process
A comprehensive search of the above-named databases yielded a total of 369 initial potentially relevant abstracts and articles. During the preliminary review of the abstracts and articles, 341 items were excluded based on the exclusion criteria. Following this, 27 articles were eligible for further evaluation. Of this number, 22 of the articles were excluded because the studies did not specifically report on nPEP. Only 5 articles met the inclusion criteria and were used for the current study. Figure 1 displays the flowchart of the selection process. The 5 articles were independently reviewed by two of the researchers (SI, OM). The researchers identified the following key themes based on literature review: socio-demographic characteristics of study sample, awareness, knowledge and use of PEP, reasons for seeking HIV nPEP, timeliness in presenting for PEP, adherence to guidelines and recommendations for nPEP by healthcare institutions, ARVs used for nPEP, side effects and adherence, monitoring and follow-up visits and strength of research evidence of the reviewed studies. These themes formed the basis for the independent review of the articles by the researchers. All information and findings obtained independently were collated and reconciled, where necessary, and the final synthesized version of the work was used for this study.
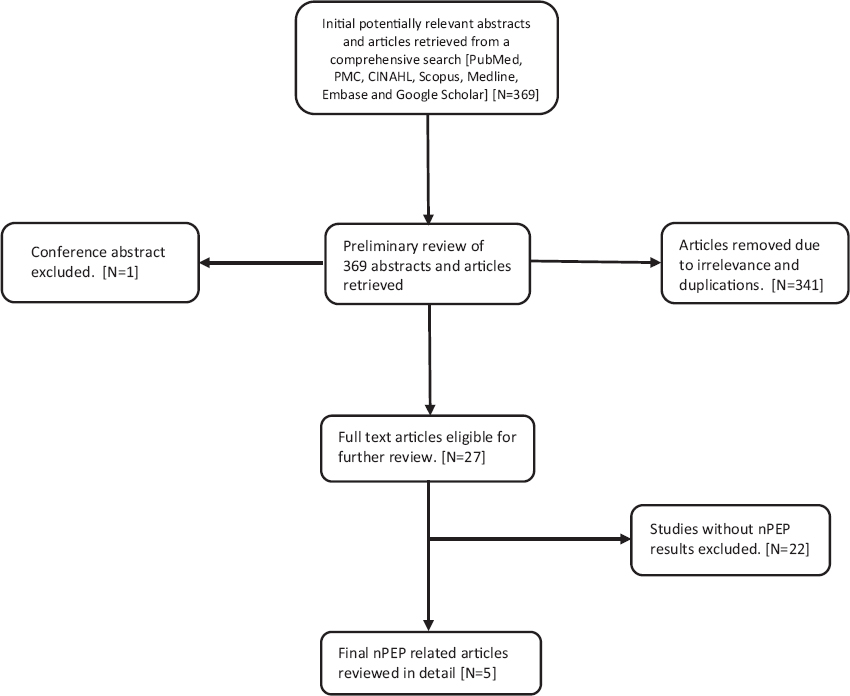
- Flowchart of nPEP Research Studies Selection Process
2.3. Types of Studies
One of the five studies reviewed was a cross sectional survey that examined the level of awareness and knowledge of PEP and PrEP among students of two Nigerian universities.41 Two of the five studies involved retrospective reviews of medical records.42,43 Onyedum et al. assessed the clinico-demographic characteristics of patients who received PEP and nPEP services from the University of Nigeria Teaching Hospital, Ituku Ozalla, between January 2007 and June 2009.42 Olowookere et al. examined the pattern of presentation and outcome of patients who were given PEP at the antiretroviral clinic, Yaba, Lagos, from January 2005 to December 2006.43 One study was a retrospective review design.44 Nwokeukwu et al. evaluated the socio-demographic characteristics and prevalent mode of exposure of patients who received PEP services and adequacy of PEP services received from September 2008 to July 2011 at the Federal Medical Center (FMC) Umuahia, in the Southeast region of Nigeria.44 One of the five studies was reported as a retrospective cohort study.45 However, on a closer examination, it lacked any control or unexposed groups to compare with the cohort nor was an absolute risk estimate performed in the study, hence it was really a retrospective review of medical records.46 Ekama et al. evaluated the nature of exposure, time of presentation and treatment outcomes of patients who utilized PEP services at the HIV treatment center of the National Institute of Medical Research, Lagos.45
3. Results
3.1. Socio-demographic Characteristics of Study Sample
In the four studies carried out in a healthcare setting, a total of 331 patients presented for nPEP services.42-45 Ajayi et al.41 surveyed a total of 748 university students to determine their level of knowledge and awareness of PEP. Table 1 shows the summary of the 5 HIV nPEP related studies conducted in Nigeria that were eligible for inclusion in this review. Across the four studies that examined exposed victims, the age of exposed victims ranged from 0 to 64 years. Two studies reported mean ages of 27.9±12.3 years43 and 29.01±7.96 years.42 Females represented 64%-78% of the exposed victims across all four studies that examined patients who presented for nPEP.42-45 This is similar to a study in nPEP that reported that 81% of individuals seeking nPEP were females.47 Ekama et al. reported that 67.2% of patients in the study had a tertiary education, 70.7% were employed and 62.1% were single.45 Olowookore et al. reported that 31.3% were students and 18.8% were civil servants.43 In the study by Ajayi et al. among university students, most of the study participants were below the age of 24, lived in off campus residencies and were Christians.41 The other four studies did not report on the residency and religion of the study participants.
| Research Study | Study design | Study objectives | Data source/study setting | Data collection period | Sample size | Results/findings |
|---|---|---|---|---|---|---|
| Onyedum et al. 201142 | Retrospective review | To evaluate the clinico-demographic characteristics of patients accessing PEP services in a tertiary health institution | Hospital: University of Nigeria Teaching Hospital, Ituku Ozalla, Enugu State (SE region) | Jan. 2007 to June 2009 | n=116 n=37* | 25.9% of exposure was due to rape. More females than males sought for the PEP services. |
| Nwokeukwu et al. 201244 | Retrospective study | To have baseline demographic information of people receiving PEP for HIV in the tertiary institution and time of reporting | Hospital: Federal Medical Centre, Umuahia, Abia State (SE region) | Sept. 2008 to July 2011 | n=120 n=64# | 77.5% reported within 24 hours of exposure; 22% were males; 46% were within the age group 21-30; There was a steady increase in the number of reporting per year (37.5% increase from January to July 2011). |
| Ajayi et al. 201841 | Cross sectional survey | To examine the level of awareness and use of PrEP and PEP among University students | University: University of Ilorin and Nasarawa State University (NC region) | Feb. to April 2018 | n=784 | Level of awareness of PEP was 25.4%; Only 5.6% and 1.5% of students had seen or used any HIV prophylaxes; Ever tested for HIV, nude exchanges, sex without condom, knowledge of partner’s HIV status were the significant determinant of awareness of PEP. |
| Ekama et al. 201745 | Retrospective cohort study | To evaluate the nature of exposure, treatment outcome, time of presentation for treatment, assess adherence to follow up visits as well as identify gaps in PEP treatment practice in the clinic. | Clinic: HIV treatment Center at Nigeria Institute for Medical Research, Lagos State (SW region) | Jan. 2006 to Oct. 2016 | n=314 n=206∆ | Majority of patients were female (73.6%); 98% presented for treatment within 72hours of exposure; Only 2% completed follow up visits. |
| Olowookere et al. 201048 | Retrospective review | To examine the pattern of presentation and outcome of clients who were given PEP at UCH, Ibadan, Nigeria. | Clinic: Antiretroviral Clinic University College Hospital, Ibadan, Oyo State (SW region) | Jan. 2005 to Dec. 2006 | n=48 n=24□ | Rape constituted 100% of the cases; 23.8% could not complete drug therapy due to side effects; 16.7% of patients did not compete follow up visit. |
3.3. Awareness, Knowledge and Prior use of PEP
Out of the five studies reviewed, only one study assessed the level of awareness, knowledge and prior use of nPEP.41 Among university students who participated in the study conducted by Ajayi et al., only 25.4% were aware of postexposure prophylaxis.41 While ever tested for HIV, nude picture exchanges, sex without condom, knowledge of partner’s HIV status were the significant determinants of awareness of PEP, awareness of PEP was not associated with sex and age.41 Students who had ever tested for HIV were one and a half times more likely to be aware of PEP compared to those who had never tested for HIV.41 Only 10.6% and 1.5% of the patients indicated that they knew where to get HIV prophylaxis (either PrEP or PEP) and had ever used them, respectively.41
3.3. Reasons for Seeking HIV nPEP
Table 2 presents the reasons for HIV non-occupational post exposure prophylaxis. Four out of five studies reported on the mode of exposure that led individuals to seek nPEP.42,44,45,48 Rape was the most frequently occurring reason for seeking nPEP (25.9% to 64.1%) in all the four studies conducted in hospital settings.42-45 This is similar to two other studies conducted in Kenya and Canada where rape accounted for 82% and 68% of non-occupational exposure respectively.49,50 A contrasting result was reported by a study carried out in Seattle, Washington were rape accounted for only 22% of nPEP exposure.51 Other reasons, as indicated in Table 2, include human bite, and blade cut.
3.4. Timeliness in Presenting for PEP
Four out of five studies reported on patient’s timeliness in seeking for nPEP after HIV exposure.42,44,45,48 Most patients across four of the studies reviewed presented for PEP within 72 hours of exposure.42,44,45,48 In the study by Ekama et al., only about 2% of exposed patients reported for PEP after 72 hours.45 In two of the studies, the majority of the exposed patients reported within 24 hours of exposure (77.5%44 and 50%42) which contrasts with one study where the majority (82%)45 presented for PEP after 48 hours, with only 6% presenting for PEP within 24 hours. Of the 10 patients who reported after 72 hours in the study by Onyedum et al., majority were sexual assault victims.42 Being male was associated with early presentation for PEP.42 We found no other study that explored this relationship between gender and early presentation for PEP.
3.5. ARVs used for nPEP, Side Effects and Adherence
Only two out of the five studies reported the type of ARVs used for nPEP for patients. Olowookore et al. reported that 56% of patients had nonnucleoside reverse transcriptase inhibitor (NNRTI)-based highly active antiretroviral (HAART).43 while Ekama et al. reported that 76% of patients were placed on the three-drug protease inhibitor (PI)-based HAART.45 Low risk patients were placed on a two-drug regimen,43,45 while patients at no risk were not given any drugs because their source of exposure was HIV negative.43 The most reported adverse effects of the drugs were nausea/vomiting, dizziness/body weakness, bad dreams/poor sleep, diarrhea, skin rash, dysuria and headache.43,45 About 23.8% of the clients could not complete the drug therapy because of these adverse effects.43 However, Onyedum et al. reported no side effects in patients who received the nPEP drug regimens.42
3.6. Monitoring and Follow-up Visits
One out of the five studies reported an 83.3% follow-up rate at the sixth month.43 In contrast, two out of the five studies42,44 reported that there was no follow-up visit by any of the patients. Ekama et al. reported that 57% of patients returned to the clinic only once and only 2% of patients completed the sixth month follow-up visits.45
3.7. Adherence to Guidelines and Recommendations for nPEP by Healthcare Institutions
Treatment guidelines
According to the National guideline for HIV Prevention Treatment and Care by the Federal Ministry of Health, Nigeria, the likelihood of the source of exposure being HIV positive, the time that has transpired since the event, and the risk associated with exposure characteristics should guide the recommendation of nPEP for individuals exposed to HIV infection and victims of sexual assault.18,52 For sexual assault victims, when the assailant’s HIV status is unknown, occurrence of vaginal or anal penetration, ejaculation on mucous membrane, involvement of multiple assailants, presence of mucous lesion on the victim or the assailant, and other predisposing characteristics of the victims must be considered in risk assessment for HIV exposure following sexual assault. For other forms of exposure, patients must be assessed to determine, if exposure was low risk or high risk (see Table 3). A three drug regimen with TDF+ 3TC (or FTC) as the preferred backbone is recommended for nPEP for adults and adolescents and must be initiated as soon as possible up to 72 hours of the assault occurring.18,52 For children less than 10 years of age, the preferred backbone for the three drug regimen for nPEP is AZT+3TC.18 It is recommended that follow up visits be slated at baseline, 2 weeks, 6 weeks, 3 months and 6 months after the event. It is also advised that patients be counseled on benefits and known toxicities of ARV, benefits of early initiation of nPEP, adherence to ARV regimen and necessary follow-up visits.18,52 Table 3 shows a summary of nPEP guidelines and recommendations by the Federal Ministry of Health in Nigeria. We assessed the practice of health care institutions where the data for the studies were collected using the following key measures culled from the National guideline for HIV Prevention Treatment and Care by the Federal Ministry of Health, Nigeria; (a) basis for treatment initiation (b) HIV exposure risk assessment (c) patient counseling, (d) ARVs used for nPEP and (e) follow up visit scheduling.
| Basis for treatment initiation | HIV exposure risk assessment | ARV regimen for nPEP | Follow-up visit schedule | Patient counseling |
|---|---|---|---|---|
| Victim is HIV negative and risk of HIV exposure is present | Occurrence of vaginal or anal penetration, ejaculation on mucous membrane, multiple assailants involved, presence of mucous lesion on the victim or assailant, predisposing characteristics of victim to HIV transmission | TDF/3TC/EFV (300/300mg/600mg) o.d. Or AZT/3TC (300/150mg) b.d+EFV (600mg) Nevirapine should never be used for PEP as the risk of fatal hepatotoxicity outweighs the risk of HIV infection. Where Efavirenz is contraindicated, either of the 2 drug combinations may be combined with ATV/r or LPV/r | Baseline, 2 weeks, 6 weeks, 3 months and 6 months | Benefits and known toxicities of ARV, benefits of early initiation of nPEP, adherence to ARV regimen, necessary follow-up visits and continued counselling |
Abbreviations: ATV/r=atazanavir/ritonavir, LPV/r=Lopinavir/ritonavir, TDF=Tenofovir, 3TC=lamivudine, AZT=Zidovudine, d4t, EFV=Efavirenz, ZDV=stavudine, IDV
Summary of adherence to guidelines and recommendations for nPEP by healthcare institutions
Table 4 summarizes the adherence of the selected healthcare institutions to nPEP guidelines and recommendations based on the studies reviewed. The selected institutions in the reviewed studies include: University of Nigeria Teaching Hospital (UNTH), Ituku Ozalla, Enugu; Antiretroviral Clinic of the University College Hospital (UCH), Ibadan, Nigeria; Federal Medical Centre (FMC), Umuahia; and HIV Treatment Centre at the Clinical Sciences Department of the Nigerian Institute of Medical Research (NIMR), Lagos. The HIV Treatment Center at the NIMR, Yaba, Lagos, followed the guideline recommendation for ARV drug regimen and follow up visit scheduling.45 The ARV Clinic at UCH, Ibadan in Oyo state, followed the guidelines and recommendations for ARV drug regimen and HIV risk assessment.43 In the study conducted at UNTH, Ituku Ozalla, Enugu, only baseline and 6 months follow-up visits were reported.42 In the study by Nwokeukwu et al.44 at FMC, Umuahia, Abia state, rape, unknown HIV status of assailant and the negative HIV status of all but one of the victims was in line with the guidelines and recommendations for treatment initiation of nPEP. None of the studies reviewed reported about patient counselling.
| Research Study | Healthcare Institution | Basis for Treatment Initiation | HIV exposure risk assessment | ARV Regimen for nPEP | Follow-up Visit Schedule | Patient Counseling | Conclusion |
|---|---|---|---|---|---|---|---|
| Ekama et al. 201745 | HIV treatment Center at NIMR Lagos State (SW region) | Rape, condom burst, unprotected sex, childbirth delivery with bare hands, human bite, and sharp objects injury | Not reported | AZT/3TC TDF/3TC | Baseline, 2 weeks, 6 weeks 3months and 6months | Not reported | The guideline for ARV regimen and follow-up scheduling was followed. It was unclear if the guidelines and recommendations for risk assessment, patient counselling and treatment initiation were followed. |
| Olowookere et al. 201048 | Antiretroviral Clinic UCH, Ibadan, Oyo State (SW region) | Rape. All victims were HIV negative before initiation of therapy | Risk assessment was carried out. High risk patients were placed on treatment. | d4t+3TC+EFV ZDV+3TC+LPV/r ZDV+3TC+EFV d4t+3TC+IDV d4t+3TC+LPV/r ZDV+3TC+IDV ZDV+3TC | Follow up at baseline and 6months reported | Not reported | The guideline for ARV regimen was followed. It was unclear if the guidelines and recommendations for risk assessment, follow-up scheduling, patient counselling and treatment initiation were followed. |
| Onyedum et al. 201142 | UNTH, Itukwu Ozalla, Enugu State (SE region) | Rape, blade cut, human bite. Some patients refused to be screened prior to PEP | Not reported | Not reported | Follow up at baseline and 6months reported | Not reported | It was unclear if the guidelines and recommendations for risk assessment, ARV regimen, patient counselling and treatment initiation were followed. |
| Nwokeukwu et al. 201244 | FMC Umuahia, Abia State (SE region) | Rape | Not reported | Not reported | Not reported | Not reported | No conclusions could be made due to lack of information |
Abbreviations: ATV/r=atazanavir/ritonavir, LPV/r=Lopinavir/ritonavir, TDF=Tenofovir, 3TC=lamivudine, AZT=Zidovudine, d4t, EFV=Efavirenz, ZDV=stavudine, IDV=Indinavir
3.8. Strength of Evidence of Reviewed Studies
d) Statistical Analysis: Two out of the five studies assessed carried out inferential statistics to determine the associations between key dependent and independent variables.41,42 Onyedum et al. carried out bivariate analysis to determine the association between clinical and sociodemographic characteristics with time of presentation for PEP.42 Ajayi et al. used logistic regression to determine the correlates of awareness of PrEP and PEP.41 Of the two studies that carried out inferential statistical analysis, only one of the studies41 carried out power analysis to determine the sample size required to estimate a meaningful effect. Three of the five studies assessed reported only descriptive statistics such as means, frequencies and percentages.43-45
4. Discussion
Findings from this review indicate that very little has been done in nPEP research in Nigeria thus leaving a large gap in the state of the science on the subject matter. As pointed out in the study by Ajayi et al., there is a general lack of awareness among young people about PEP, and lack of knowledge of where to access PEP when needed.41 This finding is consistent with reports from a 2017 National health survey, which showed that only 28.6% of young people aged 15-24 could correctly identify ways of preventing sexual transmission of HIV.54 This raises a cause for concern because young people in Nigeria are among the most vulnerable group due to several reasons including their likelihood to engage in risky sexual behavior and low HIV risk perception.4,40,55 Also young women aged 15-24 are almost twice as likely to be infected with HIV as their male counterparts in Nigeria.26 This is similar to other parts of Sub-Saharan Africa where incidence rate of HIV infections among young women aged 15-24 were significantly higher than among young men of the same age.56-58 The National HIV Strategy for Adolescents and Young People was developed as an effort to tailor scaled-up interventions specific to adolescents and young people.59 The South African National Strategic Plan has a detailed section for adolescent and young people with focus on nPEP services, youth friendly health education and literacy as part of key prevention strategy.56 Nigeria needs to emulate this comprehensive tailored guideline for its vulnerable groups especially adolescents and young people. To support policymakers to design and implement effective and sustainable HIV prevention program among her vulnerable groups, it is therefore important that knowledge gaps regarding PEP among young people in Nigeria be addressed through rigorous qualitative and quantitative research.
As indicated in 4 of the reviewed articles, sexual assault remains the top reason for non-occupational exposure to risk of HIV infection in Nigeria.42-45 In all 4 studies, most of the sexual assault victims were females.42,44,45,48 This finding is consistent with other literatures that have found that adolescent and young adult women are disproportionally affected by sexual assault in Africa24 and around the world.60 The reported high incidence of sexual assault against women in Nigeria has been noted previously as a symptom of gender inequality and gender gap.28,31,61 Gender inequalities, including gender-based violence, has been reported to exacerbate women and girls’ vulnerability to HIV and tend to block their access to HIV services.62,63 The UNAIDS Prevention Gap report, 2016, noted that Nigeria allocated less than 1% of its total HIV/AIDS budget to interventions specific to gender equality and HIV.62 An analysis of the HIV/AIDS National Strategic Plans (NSP) of Sub-Saharan African countries noted the dire need for incorporation of gender equality and sex-disaggregated targets across the region’s NSP to enable outcome monitoring and evaluation among both men and women.64 Due to societal stigmatization, survivors of sexual assault in Nigeria are sometimes reluctant to report the incidence to a health care provider or law enforcement agent leading to delay in accessing health services.11 From the perspective of HIV infection, delay is dangerous since PEP drugs must be initiated within 72 hours of exposure to HIV risk of infection to be effective.65,66 In view of this, more work needs to be done to address gender-based violence in Nigeria as part of the HIV prevention strategy. Furthermore, studies have documented depression among sexual assault survivors,36,67,68 yet none of the studies reviewed documented any mental health services options for victims of sexual assault. This reveals a huge gap in sexual assault care in the Nigerian health care system that needs to be addressed as a matter of urgency.
Follow up visits by patients who received nPEP was very low. Two of the studies reported no follow up visits.42,44 One study, however, reported that 83.3% of the patients followed up by the 6th month.43 A study in Switzerland reported that 82% presented for nPEP within 48 hours of exposure,69 while an Australian study reported a low follow up rate with only 44% presenting within 48 hours.70 It is unclear why there was such a sharp contrast between the findings by Olowookore et al.43 and the other three of five studies42,44,45 with respect to follow up. It is unclear whether this was a function of regional differences in the location where the studies were carried out, inadequate counselling of patients or due to poor record keeping by the service providers since secondary data were used in all the four studies that assessed this variable. In addition, since most of the reasons for nPEP were associated with sexual assault, it is also possible that the patients were traumatized, depressed37 or worried about confidentiality issues, especially due to the social stigma attached to rape and HIV in Nigeria.71-77 Other studies have also reported poor follow up visits in Sub-Saharan Africa47,78 and other parts of the world.51,70,79 The generally low follow-up visits rates beg for an effective intervention such as broader HIV and PEP public education, more effective counselling approaches, training in record keeping for service providers and the need to reassure patients of confidentiality.
There was insufficient data to adequately capture adherence of healthcare institutions to guidelines and recommendations. Generally, patients were initiated on treatment, if they were HIV negative, HIV status of source of exposure was unknown, and there was adequate risk of exposure.42,43,45 In the two studies that reported on the ARV given at the various healthcare institutions, the guideline in place at the time was clearly followed.43,45 The guidelines and recommendations by the Federal Ministry of Health advocates that patients be counseled on the benefits and known toxicities of ARV, benefits of early initiation of nPEP, adherence to ARV regimen and necessary follow-up.18,52 The fact that no study reported counseling services following nPEP exposes the huge gap that exist in adherence to guidelines and recommendations among the healthcare institutions in Nigeria. In part, this might help explain the reasons for low rate of follow-up visits by patients. Another explanation for the absence of patient counseling in the healthcare institution is that they may not have been recorded. Regardless of the reason for lack of reported patient counseling, healthcare providers especially pharmacists must systematically counsel patients in the key areas stipulated by the guideline, starting from the time of presentation till the completion of follow-up at six months, and indefinitely, if the patient seroconverts. This is one of the key areas that must be addressed if Nigeria plans to reach her goal of elimination of new infections by 2030.
The success of HIV PEP largely depends on strict adherence to medication regimen. Only one study reported findings relating to medication adherence among patients that received nPEP.43 About 23.8% of patients in the study discontinued their treatment due to side effects. However, the HAART combinations that these patients were adversely reacting to, the alternative therapy offered, if any, and the demographic characteristics of the patients who discontinued treatment were not reported in the study. The recent national guideline for PEP in Nigeria recommends that Stavudine be phased out80 but the study by Olowookore et al.43 was carried out retrospectively using case notes from January 2005 to December 2006, hence Stavudine was widely used in patients on a 3-drug combination. Although Ekama et al. did not document any adverse effects from the nPEP regimen given to patients, tolerability of the drugs remains to be established given the poor rate of patient follow-up visits (2%) reported.45 The other two studies did not report on the exact medications given to patients nor on medication adherence by the patients.42,44 This again, suggests that it might be a case of poor record keeping by healthcare providers and administrators and/or inadequate counselling of patients especially on the side effects of the HAART PEP regimen. The role of pharmacists here cannot be overemphasized. Pharmacists must properly counsel patients on the need to strictly adhere to medication, and to immediately report to healthcare providers any side effect they may experience to facilitate proper case management. Also, pharmacists need to educate patients on drug-drug interactions, especially as it is common for some patients to take herbal remedies while still on HAART.81,82
Nigeria faces an increasing sweep of violence ranging from killings involving herdsmen to Boko Haram insurgency resulting in millions of internally displaced individuals.83 Situations such as these are often associated with increased sexual assault and violence especially against women with grave implications for HIV non-occupational exposure.80,84-87 Furthermore, violent situations and displacement is a major barrier to access to care and other humanitarian services,83,87 which is precarious in the context of nPEP which must be initiated within 72 hours of exposure to potential HIV infection.65 Interventions tailored specifically for internally displaced persons or individuals living in areas of high violence must be designed to enable access to care.
Of the few studies that addressed non-occupational post exposure prophylaxis in Nigeria, all but one of the studies relied on retrospective data which had missing observations.42,44,45,48 Three out of the five studies were retrospective chart review and one was a retrospective cohort design.45 The study by Ekama et al. which is reported to be a retrospective cohort study, however does not have any control or unexposed groups to compare with the cohort nor was an absolute risk estimate performed in the study,46 hence, it is truly a retrospective review of medical records rather than a cohort study.46 While often quick and inexpensive to conduct, the strength of evidence of most retrospective studies is severely weakened by factors such as: information bias, recall bias, lack of control over variables collected in the data and inability to establish cause and effect.88,89 Only one study out of the five reviewed studies collected data prospectively but relied on self-reporting.41 There are many issues that arise with self-reporting including social desirability and recall bias.90,91 The study by Ajayi et al. was a thoroughly conducted cross sectional study that utilized primary data. However, cross sectional studies are often inherently limited by the fact that they are a snap shot in time and can answer prevalence questions but cannot estimate a cause and effect relationship.92 Furthermore, the sample size of patients presenting for nPEP in most of the studies limit the generalization of the respective study findings. There were also limited statistical analyses conducted in three of the studies reviewed as they relied only on basic descriptive statistics.43-45 Only one of the two studies that performed inferential statistics did a power analysis41 to ensure significant effect of the sample size. Rigorous prospective studies are needed to answer important cause-effect questions in the area of nPEP in Nigeria. Researchers conducting retrospective studies on nPEP in Nigeria must properly conceptualize their research approach and follow stringent guidelines in order to strengthen the validity of evidence derived from such studies.
4.1. Limitations and Strengths of Study
This review is limited by the fact that there are very few studies that address non-occupational post exposure prophylaxis in Nigeria. Furthermore, none of the articles reviewed were solely focused on non-occupational post exposure prophylaxis and this may have shadowed the full impact of occupational post exposure prophylaxis outcomes. Consequently, our findings on nPEP based on the current review should be interpreted with utmost caution. While this is a limitation, it serves to further highlight the importance of this review as it revealed a huge knowledge gap in the state of science of nPEP in Nigeria. Our review work is also further limited by the fact that only studies published in English language were reviewed. However, there may be some relevant studies omitted if they were published outside the time frame of this review. Accordingly, we cannot guarantee that all the literatures published on nPEP in Nigeria are included in the current review. Despite these limitations, the strength and relevance of the current study lies in being a foundational work that attempts to assess the state of science of nPEP in Nigeria. The work has helped to highlight the obvious knowledge gaps in research evidence on nPEP use and practice in Nigeria, and lay a road map of important areas to focus future research efforts on.
4.2. Public Health and Practice Implications
As observed in the study by Ajayi et al, there is low knowledge of HIV post exposure prophylaxis especially among young people.41 This implies that if the need arises for nPEP following non-occupational exposure, majority of the young people may not access needed services because they do not have the knowledge, thus potentially leading to new HIV infections that could have otherwise been prevented. The demographics of individuals affected by non-occupational exposure to potential HIV infection through sexual assault is disproportionally tilted towards women. Young women in Nigeria are twice as vulnerable to HIV infection as their male counterparts.26 This is similar to other parts of Sub-Saharan Africa where incidence rate of HIV infections among young women aged 15-24 were significantly higher than among young men of the same age.56,57 This exposes the effect of gender gap, the unequal balance of power among men and women in Nigeria, which is ranked 122 out of 144 countries in gender gap globally.93 Consequently, there is need for policy changes to strengthen the protection for women against sexual assault in Nigeria and interventions to educate more women on where and how to access needed care especially nPEP. Gender inequalities, including gender-based violence has been reported to exacerbate women and girls’ vulnerability to HIV and tend to hinder their access to HIV prevention, treatment and care services.63
Low follow up visits prevent health providers from effectively monitoring patients especially with respect to medication adherence and monitoring for possible seroconversion. This is important because antiretroviral drugs require strict adherence without which the drug will not work effectively and may lead to resistance. Better counselling by healthcare providers, especially pharmacists who serve as important point of contact in dispensing nPEP drugs, might help to improve the problem of poor follow up visits. Lack of adherence to all key areas of the guidelines and recommendations by health institutions could mar the goal of eradication of new HIV infections by 2030. The government must invest in translational research in Nigeria, to bridge the gap between research, guidelines and recommendations and the actual practice by healthcare providers.
No study was found that explored nPEP in the South-South geopolitical zone of Nigeria which has the highest HIV prevalence in Nigeria.80 Studies need to be carried out on the awareness, knowledge and pattern of HIV nPEP utilization in the different geopolitical zones of Nigeria to determine the disparities that might exist and to inform health intervention programs that will address existing gaps. Furthermore, since Nigeria is a culturally diverse country where culture and health behavior often overlap,94,95 it is important for researchers to assess how cultural differences might affect nPEP utilization across geographical regions in Nigeria. Findings from such studies will enable more culturally sensitive interventions to be planned and implemented, where necessary.
Other factors that affect nPEP services in Nigeria include, poor accounting in disbursement of HIV/AIDS funding, noncompliance96,97 and violence and insurgency.80 Use of obsolete accounting software and technology makes it difficult to adequately audit disbursed HIV funding thus leaving room for inappropriate handling of funds. To prevent this, regular audit of funding must be carried out by internal and external auditors and obsolete accounting tools should be replaced with modern accounting software and tools that can track and monitor financial disbursements in real time. This is important because, without putting in place the proper structure, the national strategic framework will simply not work as intended.
In order to achieve the goal of eradicating new infections in Nigeria by 2030,80 the federal government of Nigeria must effectively implement and enforce policies where necessary, and ensure that HIV prevention interventions are carefully planned and tailored to target high-risk groups in other to increase knowledge, awareness and eradicate barriers to access HIV prophylaxis. Also, healthcare providers must continuously undergo training to adapt to the changing treatment, care and prevention needs of patients thereby improving their practice. In addition, HIV specialists and researchers from academic medical centers or urban clinics can use video conferencing technology to provide real-time clinical expertise and support to providers in the rural areas. This approach could enhance the reach and allow many Nigerians gain access to available and necessary nPEP services could help reduce the transmission of HIV.
4.3. Global Health Implications
With a population of over 195 million persons, Nigeria is the most populous country in Africa98 and among the most populous countries in the world. About 1.9 million Nigerians out of 36.9 million persons globally, are currently living with HIV.5 This makes Nigeria one of the worst hit countries by HIV. Due to its regional status and high HIV epidemic, it serves as an important epicenter in the fight against HIV in Africa and continues to receive funding and technical support for research in the area of HIV prevention. In view of this, the paucity of research on nPEP in HIV prevention in Nigeria is worrisome as nPEP has been included by UNAIDS as part of the global strategy to prevent HIV especially among adolescent girls and young women.99 The Fast-Track targets for HIV prevention and treatment which includes a 75% reduction in new HIV infections globally by 2020 as compared to 2010,100 can only be achieved with tailored interventions informed by adequate research. Prevention of new HIV infections is very important especially in low income countries like Nigeria because increased incidence rates can lead to significant drain on resources available for the elimination of AIDS as a public health threat. For Nigeria which depends largely on international funding for its HIV response,101,102 the situation is dire as global HIV funding for middle and low-income countries continue to reduce.103 To meet up to global prevention goals for HIV, Nigeria’s HIV AIDS Strategic Plan must be updated to include sex-disaggregated data and tailored responses to key groups in a manner similar to South Africa’s NSP56; Nigerian Health care providers must be continually trained to give quality care to individuals seeking nPEP services; and more studies on nPEP must be carried out in a rigorous manner to strengthen the body of research evidence available to inform HIV prevention policies and intervention programs in Nigeria.
4.5. Conclusions
The state of the science regarding nPEP in Nigeria is still at the developmental stage with most of the research evidence on nPEP considered weak following the sample size, study design and analytical approach involved. We noted the existence of low awareness of PEP and inadequate knowledge of where and how to access it among college students.41 Although our findings cannot be generalized, the study points to an obvious knowledge gap in HIV prevention efforts that needs to be addressed among this subpopulation. Sexual assault was identified as the major reason for non-occupational exposure to risk of HIV infection in Nigeria. There was late presentation for PEP and poor follow-up visit rates among exposed victims in most of the studies reviewed. Since all studies included both occupational and non-occupational post exposure prophylaxis, our findings on nPEP based on the current review must be interpreted cautiously. For nPEP to have a population-level impact on HIV prevention, nPEP education and promotion must be intensified and targeted especially towards young adolescent females who are the most vulnerable group to sexual assault. It is recommended that a rigorous and comprehensive research study or a national study using a large sample size be conducted on nPEP in Nigeria, and efforts made in such studies to focus on the themes identified in this review including the determinants of nPEP services utilization, and adherence to the national guidelines and recommendations on PEP by the healthcare providers.
Acknowledgment
The authors thank the authors of the articles used for this review.
Conflict of Interest: The authors declare that there are no conflicts of interest related to research, authorship, and/or publication of this article.
Funding/Support: None.
Ethics Approval: The study was a systematic review of published articles and did not require a review by an Institutional Review Board.
References
- Global Health Observatory data repository. http://apps.who.int/gho/data/view.main.22100WHO?lang=en
- 2018. Global HIV Statistics. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
- Nigeria HIV/AIDS Indicator and Impact Survey 2019. https://naca.gov.ng/naiis-national-summary-sheet/
- Revised National HIV and AIDS Strategic Framework 2019-2021. https://naca.gov.ng/revised-national-hiv-and-aids-strategic-framework-2019-2021/
- Framework for action in the WHO African Region, 2016 - 2020. Regional Office for Africa: World Health Organization; http://www.who.int/iris/handle/10665/259638 2017
- Economic Burden of HIV/AIDS Infection, Stigmatization and Productivity Loss:Empirical Evidences from Gwagwalada, FCT-Nigeria. Research and Analysis Journal 2019:86-102.
- [Google Scholar]
- The economic burden of HIV and AIDS on households in Nigeria. African Journal of AIDS Research. 2009;8(1):107-114.
- [Google Scholar]
- Assessing the economic impact of HIV/AIDS on Nigerian households:a propensity score matching approach. AIDS. 2008;22:S95-S101.
- [Google Scholar]
- Impact of HIV/AIDS on economic growth and development in Nigeria. AIDS on Economic Growth and Development in Nigeria (April 25 2013). https://ssrn.com/abstract=2695373 or http://dx.doi.org/10.2139/ssrn.2695373
- [Google Scholar]
- 2018. Global Information and Education on HIV and AIDS. https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/nigeria
- MMWR Morbidity and mortality weekly report. 2016;65(17):458.
- A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. The New England Journal of Medicine. 1997;337(21):1485-1490.
- [Google Scholar]
- Adherence to Post-Exposure Prophylaxis (PEP) and Incidence of HIV Seroconversion in a Major North American Cohort. PloS One. 2015;10(11):e0142534.
- [Google Scholar]
- Animal studies of prophylaxis. The American Journal of Medicine. 1997;102(5):39-44.
- [Google Scholar]
- Postexposure prophylaxis with zidovudine suppresses human immunodeficiency virus type 1 infection in SCID-hu mice in a time-dependent manner. Journal of Infectious Diseases. 1991;163(3):625-627.
- [Google Scholar]
- Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposure to HIV in the United States:recommendations from the U.S. Department of Health and Human Services. MMWR Recommendations and reports:Morbidity and Mortality Weekly Report Recommendations and Reports. 2005;54((Rr-2)):1-20.
- [Google Scholar]
- National AIDS and STI's Control Programme. ;2016:131-133.
- Knowledge and practice of post-exposure prophylaxis (PEP) against HIV infection among health care providers in a tertiary hospital in Nigeria. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill 2002). 2012;11(3):179-183.
- [Google Scholar]
- Knowledge, attitude and practices of HIV post exposure prophylaxis amongst health workers in Lagos University Teaching Hospital. The Pan African Medical Journal. 2014;19:172.
- [Google Scholar]
- Percutaneous injuries and accidental blood exposure in surgical residents:awareness and use of prophylaxis in relation to HIV. Nigerian Journal of Clinical Practice. 2011;14(1):34-37.
- [Google Scholar]
- Awareness and practice of safety precautions among healthcare workers in the laboratories of two public health facilities in Nigeria. The Nigerian Postgraduate Medical Journal. 2011;18(2):141-146.
- [Google Scholar]
- Determinants of appropriate knowledge on human immunodeficiency virus postexposure prophylaxis among professional health-care workers in Sokoto, Nigeria. Journal of Family Medicine and Primary Care. 2018;7(2):340-345.
- [Google Scholar]
- Nonoccupational postexposure prophylaxis for human immunodeficiency virus in Sub-Saharan Africa:a systematic review. Journal of Forensic Nursing. 2011;7(2):89-96.
- [Google Scholar]
- A prospective study of post-exposure prophylaxis following sexual assault in South Africa. Paper presented at 12th Conference on Retroviruses and Opportunistic Infections 2005:25.
- [Google Scholar]
- UNAIDS. Nigeria: Country Factsheets; http://www.unaids.org/en/regionscountries/countries/nigeria/
- Prevalence and pattern of rape among girls and women attending Enugu State University Teaching Hospital, southeast Nigeria. International Journal of Gynaecology and Obstetrics:the Official Organ of the International Federation of Gynaecology and Obstetrics. 2015;130(1):10-13.
- [Google Scholar]
- Sexual assault in Lagos, Nigeria:a five year retrospective review. BMC Women's Health. 2014;14(1):115.
- [Google Scholar]
- Family background, sexual behaviour, and HIV/AIDS vulnerability of female street hawkers in Lagos metropolis, Nigeria. International Social Science Journal. 2005;57(186):687-698.
- [Google Scholar]
- Sexual assault against women at Osogbo southwestern Nigeria. Nigerian Journal of Clinical Practice. 2012;15(2):190-193.
- [Google Scholar]
- Trends and patterns of sexual assaults in Lagos south-western Nigeria. The Pan African Medical Journal. 2016;24
- [Google Scholar]
- The pattern and characteristics of sexual assault perpetrators and survivors managed at a sexual assault referral centre in Lagos. African Journal of Primary Health Care & Family Medicine. 2018;10(1):e1-e5.
- [Google Scholar]
- Prevalence and pattern of sexual assault in Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. The Pan African Medical Journal. 2016;24:332.
- [Google Scholar]
- A novel ED-based sexual assault centre in western Kenya:description of patients and analysis of treatment patterns. Emergency Medicine Journal. 2011;28(11):927-931.
- [Google Scholar]
- Substance abuse and behavioral correlates of sexual assault among South African adolescents. Child Abuse & Neglect. 2004;28(6):683-696.
- [Google Scholar]
- “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, & Abuse. 2018;19(5):512-527.
- [Google Scholar]
- Sleep disorder, depression and suicidality in female sexual assault survivors. Crisis:The Journal of Crisis Intervention and Suicide Prevention. 2000;21(4):163-170.
- [Google Scholar]
- The cost of providing comprehensive HIV treatment in PEPFAR-supported programs. AIDS (London, England). 2011;25(14):1753-1760.
- [Google Scholar]
- The lifetime medical cost savings from preventing HIV in the United States. Medical Care. 2015;53(4):293-301.
- [Google Scholar]
- HIV risk perception and constraints to protective behaviour among young slum dwellers in Ibadan, Nigeria. Journal of Health, Population, and Nutrition. 2007;25(2):146-157.
- [Google Scholar]
- Awareness and use of pre-exposure and postexposure prophylaxes among Nigerian university students:Findings from a cross-sectional survey. Medicine. 2018;97(36):e12226.
- [Google Scholar]
- HIV Postexposure Prophylaxis (PEP) in a Nigerian Tertiary Health Institution. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill 2002). 2011;10(3):171-175.
- [Google Scholar]
- Human immunodeficiency virus postexposure prophylaxis at IBadan, Nigeria. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill 2002). 2010;9(3):187-190.
- [Google Scholar]
- Human Immune Deficiency Virus (HIV) Post Exposure Prophylaxis in a Tertiary Institution, South East Zone, Nigeria. Articles from the 13 th World Congress on Public Health. April 23-27. Addis Ababa (Ethiopia) 2012:327-331.
- [Google Scholar]
- Pattern and Rate of Occupational and Non-Occupational Exposures:The Experience of a Major HIV Treatment Centre in Nigeria. Journal of Advances in Medicine and Medical Research. 2017;23(12):1-7.
- [Google Scholar]
- Distinguishing case series from cohort studies. Annals of Internal Medicine. 2012;156(1 Pt 1):37-40.
- [Google Scholar]
- The structure and outcomes of a HIV postexposure prophylaxis program in a high HIV prevalence setup in western Kenya. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2009;51(1):47-53.
- [Google Scholar]
- Human immunodeficiency virus postexposure prophylaxis at Ibadan, Nigeria. Journal of the International Association of Physicians in AIDS Care. 2010;9(3):187-190.
- [Google Scholar]
- The Structure and Outcomes of a HIV Postexposure Prophylaxis Program in a High HIV Prevalence Setup in Western Kenya. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2009;51(1):47-53.
- [Google Scholar]
- HIV non-occupational postexposure prophylaxis in a Canadian province:treatment completion and follow-up testing. International Journal of STD & AIDS. 2010;21(9):617-621.
- [Google Scholar]
- Non-Occupational Post-Exposure Prophylaxis for HIV:10-Year Retrospective Analysis in Seattle, Washington. PloS ONE. 2014;9(8):e105030.
- [Google Scholar]
- National AIDS and STI's Contro Programme. Federal Ministry of Health Abuja 2010:48-52.
- National Guidelines for HIV Prevention Treatment and Care. Nigeria: FMOH Abuja; 2016.
- Multiple Indicator Cluster Survey 2016-17, Survey Findings Report, Nigeria. https://www.unicef.org/nigeria/reports/multiple-indicator-cluster-survey-2016-17-mics
- A Cross Sectional Study on HIV Risk Perception and Sexual Behaviours among Commercial Motorcyclists in Makurdi, Benue State Nigeria. Mediterranean Journal of Social Sciences. 2017;8(3):27-33.
- [Google Scholar]
- SANAC South Africa's national strategic plan for HIV, TB and STIs 2017-2022. 2017.
- UNAIDS Communities at the Centre Defending Rights Breaking Barriers Reaching People With HIV Services. Vol 316. Geneva: Joint United Nations Programme on HIV/AIDS; 2019.
- Adolescent girls and young women:key populations for HIV epidemic control. Journal of the International AIDS Society. 2015;18(2 Suppl 1):19408.
- [Google Scholar]
- National HIV Strategy For Adolescents and Young People 2016-2022. https://naca.gov.ng/national-hiv-strategy-adolescents-young-people/
- A global overview of gender-based violence. International Journal of Gynecology & Obstetrics. 2002;78(S1):5-14.
- [Google Scholar]
- Rape in Nigeria:a silent epidemic among adolescents with implications for HIV infection. Global Health Action. 2014;7:25583.
- [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Accessed at https://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf
- Gender-based violence and HIV:Reviewing the evidence for links and causal pathways in the general population and high-risk groups. American Journal of Reproductive Immunology. 2013;69:20-26.
- [Google Scholar]
- HIV/AIDS National Strategic Plans of Sub-Saharan African countries:an analysis for gender equality and sex-disaggregated HIV targets. Health Policy and Planning. 2017;32(10):1361-1367.
- [Google Scholar]
- 2018. Focus on key populations in national HIV strategic plans in the WHO African Region. Regional Office for Africa: World Health Organization; https://apps.who.int/iris/bitstream/handle/10665/275494/WHO-AF-CDS-HIV-02.2018-eng.pdf?ua=1
- Sleep-disordered breathing, psychiatric distress, and quality of life impairment in sexual assault survivors. The Journal of Nervous and Mental Disease. 2002;190(7):442-452.
- [Google Scholar]
- The effectiveness of mental health interventions for adult female survivors of sexual assault:A systematic review. Aggression and Violent Behavior. 2015;25:15-25.
- [Google Scholar]
- Nonoccupational HIV post-exposure prophylaxis:a 10-year retrospective analysis. HIV Medicine. 2010;11(9):584-592.
- [Google Scholar]
- Non-occupational post-exposure prophylaxis in Victoria, Australia:responding to high rates of re-presentation and low rates of follow-up. International Journal of STD & AIDS. 2011;22(12):714-718.
- [Google Scholar]
- Prevalence and Psychosocial Consequences of Rape in Jos, North–Central Nigeria. International Journal of Clinical Psychiatry and Mental Health. 2017;5:11-19.
- [Google Scholar]
- Perceptions of the Social Consequences of Rape in Ezinihitte-Mbaise, Imo State, Nigeria. American Journal of Humanities and Social Sciences Research (AJHSSR). 2018;2(8):1-8.
- [Google Scholar]
- Perception of victims of rape and perception of gender social roles among college students in Southwest Nigeria:validation of a 5-item gender scale. International Journal of Adolescent Medicine and Health 2017
- [Google Scholar]
- Taming the rape scourge in Nigeria:issues and actions. Gender and Behaviour. 2016;14(3):7764-7785.
- [Google Scholar]
- HIV/AIDS related stigma and discrimination against PLWHA in Nigerian population. PloS ONE. 2015;10(12):e0143749.
- [Google Scholar]
- Knowledge gap about HIV/AIDs and stigma associated beliefs in an urban Community in Southwest Nigeria:Implication for social work. Research Journal of Health Sciences. 2015;3(4):293-302.
- [Google Scholar]
- HIV-stigma in Nigeria:review of research studies, policies, and Programmes. AIDS Research and Treatment 2017:1-13.
- [Google Scholar]
- Sexual Assault and HIV Postexposure Prophylaxis at an Urban African Hospital. AIDS patient care and STDs. 2017;31(6):255-260.
- [Google Scholar]
- A mixed methods study of non-occupational post-exposure prophylaxis at an STI clinic in Singapore:Five-year retrospective analysis and providers' perspectives. PloS ONE. 2018;13(8):e0202267.
- [Google Scholar]
- Federal Republic of Nigeria
- Evaluation of the frequency of use of herbal drugs with concomitant administration of highly active antiretroviral therapy and its effect on medication adherence in two health care facilities in south western Nigeria. Journal of AIDS and HIV Research. 2017;9(1):8-16.
- [Google Scholar]
- Widespread use of herbal medicines by people living with human immunodeficiency virus and contamination of herbal medicines with antiretrovirals in Nigeria. International Journal of STD & AIDS. 2019;30(4):371-377.
- [Google Scholar]
- Boko Haram insurgency:implications for public health. Vol 385. 2015. p. :941.
- Sexual Violence-Related Pregnancy Among Internally Displaced Women in an Internally Displaced Persons Camp in Northeast Nigeria. Journal of Interpersonal Violence 2018 doi:10.1177/0886260518792252. [Epub ahead of print
- [Google Scholar]
- Insecurity and sexual rights violations of the female minors in internally displaced camps in Nigeria. The Journal of Sexual Medicine. 2016;13(5):231-232.
- [Google Scholar]
- Internal displacement in Nigeria and the case for human rights protection of displaced persons. Journal of Policy & Globalization. 2016;51:26.
- [Google Scholar]
- Observational studies:cohort and case-control studies. Plastic & Reconstructive Surgery. 2010;126(6):2234-2242.
- [Google Scholar]
- Observational research methods Research design II:cohort, cross sectional, and case-control studies. Emergency Medicine Journal. 2003;20(1):54-60.
- [Google Scholar]
- Faking it:social desirability response bias in self-report research. Australian Journal of Advanced Nursing, The. 2008;25(4):40-48.
- [Google Scholar]
- Study design, precision, and validity in observational studies. Journal of Palliative Medicine. 2009;12(1):77-82.
- [Google Scholar]
- Why culture matters in health interventions:Lessons from HIV/AIDS stigma and NCDs. Health Education & Behavior. 2014;41(1):78-84.
- [Google Scholar]
- Using a cultural framework to understand factors influencing HIV testing in Nigeria. International Quarterly of Community Health Education. 2016;37(1):33-42.
- [Google Scholar]
- 2015. The Global Fund Updates:Investigation in Nigeria. https://www.theglobalfund.org/en/oig/updates/2016-05-03-investigation-in-nigeria/
- Between progress, stasis and reversals:an analysis of the Millennium Development Goals in Nigeria Paper presented at Did the Millennium Development Goals Work? Meeting Future Challenges with Past Lessons, Policy Press. 2017;Ch 13:309-334.
- [Google Scholar]
- 2017. HIV prevention 2020 road map—accelerating HIV prevention to reduce new infections by 75%. Geneva: UNAIDS; https://unfpa.org/sites/default/files/pub-pdf/hiv-prevention-2020-road-map_en.pdf
- The impact of the US president's emergency plan for AIDS relief (PEPFAR) HIV and AIDS program on the Nigerian health system. The Pan African Medical Journal. 2016;25:143.
- [Google Scholar]
- Impact of global health governance on country health systems:the case of HIV initiatives in Nigeria. Journal of Global Health. 2015;5(1):010407.
- [Google Scholar]
- 2019. Donor government funding for HIV in low-and middle-income countries in 2018. Menlo Park, CA: The Henry J Kaiser Family Foundation &UNAIDS; http://files.kff.org/attachment/Report-Donor-Government-Funding-for-HIV-in-Low-and-Middle-Income-Countries-in-2018





