Translate this page into:
Non-Occupational HIV Post-exposure Prophylaxis: A 10-Year Retrospective Review of Data Following Sexual Exposure From Yaounde Central Hospital, Cameroon
*Corresponding author email: ngwayuclaude1@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Human Immunodeficiency Virus (HIV) post exposure prophylaxis (PEP) consists of administering antiretroviral therapy within 72 hours of viral exposure and continued for four weeks. PEP has been shown to be an important means of preventing and decreasing the number of new HIV infections in the general population. The purpose of this study was to describe the profile of patients who consulted at the HIV/AIDS Care and Treatment Center of the Yaounde Central Hospital (YCH) for PEP following non-occupational exposure to HIV. To attain our objective, we carried out a 10-year retrospective review of patient records of all persons who consulted for accidental HIV exposure at the YCH, Cameroon.
Methods:
This study was an observational, retrospective analysis of hospital records of persons who consulted for PEP following accidental exposure to HIV in the outpatient HIV clinic at YCH between January 2007 and December 2016. Data extracted from patients’ records were: type of HIV exposure, sex, age, profession, level of education, HIV status of source and time to consultation. Descriptive and inferential statistics were analyzed using STATA IC 12.0. Results were presented as median and interquartile range for continuous variables. Categorical variables were expressed as frequencies and proportions.
Results:
There were 628 consultations for PEP of which 48% (299/628) were as a result of non-occupational post exposure prophylaxis (nPEP). Of those who consulted for HIV PEP following non-occupational exposure, 78% (234/299) were females; adolescents group (15-19 years) and young adults group (20 – 24yrs.) constituted 41% (125/299). Forty percent (1208/299) were secondary or high school students (level of education) and 88% (262/299) were non-healthcare workers. The median time-to-consultation for non-occupational PEP (nPEP) was 19 hours (IQR: 12.4-25.0) and HIV status of the source was unknown in 64% (191/299) of cases and positive for 8% (25/299) of cases. The most frequent indications for consulting were sexual assault, 75% (224/299); condom slippage or breakage, 10% (30/299); and unprotected consensual sexual intercourse, 15% (45/299).
Conclusion and Global Health Implications:
Consultations for nPEP are as frequent as those occupational PEP (48% vs 52% in this study) in clinical practice at YCH. A good history of the source is important as it prevents unnecessary prescriptions of ART (which themselves have potential side effects) for persons consulting for potential HIV non-occupational exposure. In our study, we found that 27% (82/299) unnecessary ART prescriptions were avoided by determining that the exposure source person had negative HIV status. In addition, adolescent or young females consulting for nPEP in clinics could be potential victims of sexual assault or gender-based violence. Where possible, we recommend that clinicians consider the source of suspected viral exposure in clinical practice prior to administering ART for PEP.
Keywords
Human immunodeficiency virus
Yaounde Central Hospital (Hôpital Central Yaoundé)
Post-exposure prophylaxis
Cameroon
Sexual exposure
Non-occupational post exposure prophylaxis
HIV
PEP
nPEP
AIDS
1. Background and Objectives
Human Immunodeficiency virus (HIV) infection is a major public health concern around the world, especially in resource-limited countries; with several modes of transmission but sexual transmission is the primary mode.1 The virus which is present in genital secretions can be transmitted during unprotected sexual intercourse with an infected partner or during an accidental breakage of the condom.2 A combination of measures and efforts are needed to end the HIV epidemic.3 These measures will include access to highly active antiretroviral therapy (HAART) for treatment and as prevention (the concept of treatment as ‘treatment as prevention’), strategies to enable and promote sustained behavioral change and adoption of healthy lifestyles, promotion of proper condom use, and the search for an effective vaccine.
Post-exposure prophylaxis (PEP) is the administration of HAART within 72 hours of accidental exposure to HIV and continued for 28 days to prevent transmission and establishment of the infection.1 The probability of HIV transmission depends on the type of exposure and the viral load of the source with the susceptibility of the exposed persons. HIV post-exposure prophylaxis is recommended when the risk of transmission is greater than 1/1000 and should be considered when the risk is between 1/1000 and 1/10,000. When the risk of transmission is less than 1/10 000, prophylaxis is not recommended.4
In Cameroon, primary HIV infection prevention strategies focus on promoting behavioral changes such as abstinence or delaying age of first intercourse, correct condom use, and fidelity to a partner for stable couples. Despite these efforts, sexual exposure to HIV is frequent and remains a public health problem in Cameroon.2 In addition, despite research pointing to the efficacy of PEP in prevention of HIV transmission, many countries of sub-Saharan Africa (including Cameroon) still face challenges in the proper implementation of PEP programs. Most people in these countries are not aware of this possibility.4
The Yaoundé Central Hospital (YCH) was the first accredited HIV/AIDS management center in Cameroon. It is a very busy health facility and cares for about 11,000 persons living with HIV (PLWHIV). On a regular basis, the hospital receives several people consulting for accidental exposure to HIV from the cosmopolitan and diverse city populations. Our hospital is considered the technical arm of the Cameroon Ministry of Public Health (MoH). Therefore, we believe that a review of PEP, especially non-occupational PEP, might help to inform national policy on the need to valorize PEP. The objective of this study was to describe the epidemiological profile of people consulting for PEP following non-occupational accidental exposure to HIV. Specifically, we described the trend over 10 years and demographic profile (age, sex, profession, level of education) of persons consulting for nPEP. We also described the type of non-occupational HIV exposure that prompted consultation, describe the HIV status of the source persons and estimate the median time to consultation following exposure.
2. Methods
2.1. Study Design and Setting
This study was an observational, retrospective study of hospital records of persons who consulted for PEP following accidental exposure to HIV in outpatient HIV clinic of the YCH between January 2007 and December 2016. At-risk exposure was defined as unprotected intercourse (receptive or insertive) with ejaculation and scenarios where mucous membrane or non-intact skin came into contact with blood or other infectious body fluids. Yaoundé is a cosmopolitan city and the capital of Cameroon. It is the second largest city after Douala with an estimated population of more than 2.500.000 persons.5 The HIV outpatient clinic of the YCH is the first ever accredited and reference clinic for HIV/AIDS management. Together with other approved HIV treatment centers it serves the population of Yaoundé. It currently cares for 11.000 PLWHIV. Cases of accidental exposure to HIV are received at night and during the weekend through emergency unit are usually referred to the clinic for management. The target population was patients who consulted for PEP following accidental exposure to HIV in outpatient HIV clinic of the YCH. We included in our study all records of patients who consulted for PEP following accidental exposure to HIV in outpatient HIV clinic of the YCHbetween January 2007 and December 2016. Records with incomplete, missing or illegible information about the type of PEP consultation (occupational or non-occupational) were excluded.
2.2. Sampling Method
A non-probabilistic consecutive sampling was employed to select patient records beginning from January 2007 to December 2016. Therefore, any record that met study criteria was included. The sample size was obtained using the following formula.
Where p is the proportion of patients consulting for PEP, ε the margin of error acceptable. We considered p=0.5 (50%) which makes it possible to obtain a maximum sample size; a precision ε = 0.05 (5%), and α = 0.05; and the critical value resulting from the normal law was therefore $$$ = 1.96. Applying this formula, the required sample size was 384, however, our study sample size was 628.
= 1.96. Applying this formula, the required sample size was 384, however, our study sample size was 628.
2.3. Study Variables
The variables of our study sex (male or female), age to the nearest completed years (which was further transformed into categories: children: < 15 years; adolescents: 15-19 years; young adult: 20-24 years; adult: 25-49 years and old: 50+ years), level of education (as a categorical variable: none or primary education, Secondary or high school education and Higher or university education), profession (none, student, non-healthcare job, healthcare job), type of exposure (needle stick injury, sexual assault, unprotected intercourse, condom breakage or slippage, mucous membrane exposure to biological fluid, exposure to blood), HIV serology status of the source person and of the exposed person (categorized as either unknown, positive or negative) and the estimated time (in hours) to consultation following an incident.
For exposed patients with a confirmed negative HIV serology, PEP consisted of either Zidovudine (ZDV) 300 mg and Lamivudine (3TC) 150 mg twice daily or a fixed-dose combination Tenofovir (TDF) 600mg and Lamivudine (3TC) 300mg once daily plus a fixed dose of either Lopinavir (LPV) 400 mg and Ritonavir (RTV) 100 mg twice a day. Exposed persons who tested were directed to begin HAART if eligibility criteria were met and the person was ready. This was the case before the World Health Organization (WHO) recommendation to treat all, irrespective of clinical or immunological stage, came into force in Cameroon. PEP was discontinued in persons who had their source later screened negative for HIV tested.
2.4. Data Collection Tools/Technique
A questionnaire developed for this study was used to collect data. The questionnaire was made of a section to collect socio-demographic information (sex, age, level of education, occupation), clinical data (cause of exposure, HIV serology of patients and cause and the estimated time to consultation). The technique of the data collection was through a review of patient records if eligibility was met for the study from which the information was collected to complete the questionnaire by the investigator. Two state registered nurses working in the unit were trained and helped in the data collection. Data was collected from October 2017 to February 2018 (five months).
2.5. Statistical Analysis
Data collected were coded and entered into Microsoft Excel. They were then transferred and analyzed using STATA IC 12.0 (Stata Corporation, College Station, TX, USA) software. Descriptive (non-inferential statistics) analysi was conducted. Categorical variables were expressed as frequencies and proportions while median and interquartile range was used for continuous variables. Inferential statistics was not used in analysis because descriptive analysis of trends and PEP and profile of persons seeking HIV PEP services was the objective. Ethical approval for the study was obtained from the Ethics Committee of Yaoundé Central Hospital (reference N° 2016/0431/CE/D/HCY). Administrative clearance was obtained from the hospital authorities and the head of service of HIV/AIDS Care and Treatment Center. Patient consent was waived for the study because it was a non-interventional study involving retrospective review of records only. However, confidentiality was respected in treating patients’ records. No data that could make identification of patients was collected.
3. Results
3.1. Trends in PEP Consultations
Between January 2007 and December 2016, 628 consultations for potential HIV exposure were recorded. A steady decline was observed in consultations for HIV exposure from 72 in 2007 to 37 in 2012 (49% decline) followed by a slight increase from 2013 to 2016 (Figure 1). Of these, 329 (52%) occurred in the healthcare setting (occupational exposure) while 299 (48%) were outside the healthcare setting (non-occupational exposure, nPEP). Four hundred and one of these consultations were eligible to receive PEP (52% nPEP and 48% occupational PEP). Ineligibility for receiving PEP were seeking care after 72 hours of incident (6 persons), identified source was screened HIV negative (213 persons), exposed person was screened HIV positive (8 persons) and started on anti-retroviral therapy. Overall, 368 persons were documented to have received PEP in the final analysis because 33 of the eligible persons had missing or un-extractable information (Table 1). Generally, males constituted 70% (432/628) of those who sought PEP services compared to females. The median age was 28 years (IQR 23-35 years) with the adult age group (25-49years) most affected. The median time-to-consultation was 16 hours (IQR: 11-23) following exposure and sexual assault was the most frequent reason for PEP prescription. In two hundred and two cases (55%) the HIV status of the source was unknown. Fifty-one percent (51%) of those who received PEP worked in the healthcare sector and the majority (68%) had high school or university education.

- Study flow chart
| Characteristic | General | Received PEP |
|---|---|---|
| (n=628) | (n=368) | |
| Non-occupational exposure | ||
| Yes | 299 (48%) | 184 (50%) |
| No | 329 (52%) | 184 (50%) |
| Missing | 0 (0%) | 0 (0%) |
| Time to consultation in hours: median (IQR) | 15.4 (11-23) | 16 (11-23) |
| Sex | ||
| Male | 432 (69%) | 258 (70%) |
| Female | 178 (28%) | 108 (29%) |
| Missing | 18 (3%) | 2 (1%) |
| Age in years: median (IQR) | 28 (23-35) | 28 (23-35) |
| Age group | ||
| < 15 years (pediatric population) | 15 (2%) | 8 (2%) |
| 15 to 19 years (adolescents) | 57 (9%) | 34 (9%) |
| 20 to 24 years (young adults) | 122 (19%) | 67 (18%) |
| 25 to 49 years (adults) | 390 (62%) | 234 (64%) |
| 50+ years (older adults) | 29 (5%) | 16 (4%) |
| Missing | 15 (2%) | 9 (2%) |
| Exposure type | ||
| Needle stick injury | 144 (23%) | 80 (22%) |
| Sexual assault | 224 (36%) | 138 (38%) |
| Unprotected intercourse | 30 (5%) | 22 (6%) |
| Condom breakage/slippage | 45 (7%) | 24 (7%) |
| Exposure to other body fluids | 169 (27%) | 94 (26%) |
| Exposure to blood | 16 (3%) | 10 (3%) |
| Profession | ||
| None | 16 (3%) | 13 (4%) |
| Non-healthcare job | 263 (42%) | 155 (42%) |
| Healthcare job | 333 (53%) | 188 (51%) |
| Missing | 16 (3%) | 12 (3%) |
| Level of education | ||
| None or primary education | 45 (7%) | 27 (7%) |
| Secondary or high school education | 121 (19%) | 78 (21%) |
| Higher or university education | 446 (71%) | 250 (68%) |
| Missing | 16 (3%) | 13 (4%) |
| Source reported HIV status at baseline | ||
| Unknown | 236 (38%) | 202 (55%) |
| Positive | 178 (28%) | 166 (45%) |
| Negative¦ | 214 (34%) | 0 (0%) |
3.2. Profile of Persons Consulting for Non-occupational Exposure (nPEP)
Of those who consulted for HIV PEP following non-occupational exposure: 78% (234/299) were females, adolescents group (15-19 years) and young adults group (20 – 24yrs.) constituted a total 41% (125/299). Forty percent 40% (120/299) were secondary or high school students (level of education) and 88% (262/299) were not non-healthcare workers (Table 2).
| Characteristic | General | Received PEP |
|---|---|---|
| (n=299) | (n=184) | |
| Sex | ||
| Male | 55 (18%) | 33 (18%) |
| Female | 234 (78%) | 151 (82%) |
| Missing | 10 (3%) | 0 |
| Time to consultation in hours: median (IQR) | 18.5 (12-26) | 19 (12.4-25) |
| Age group | ||
| < 15years (pediatric population) | 12 (4%) | 6 (3%) |
| 15 to 19 years (adolescents) | 49 (16%) | 30 (16%) |
| 20 to 24 years (young adults) | 76 (25%) | 44 (24%) |
| 25 to 49 years (adults) | 149 (50%) | 96 (52%) |
| 50+ years (older adults) | 7 (2%) | 5 (3%) |
| Missing | 6 (3%) | 3 (2%) |
| Age in years: median (IQR) | 19 (12-26) | 19 (12-25) |
| Exposure type | ||
| Sexual assault | 224 (75%) | 138 (75%) |
| Unprotected consensual intercourse | 30 (10%) | 22 (12%) |
| Condom breakage/slippage | 45 (15%) | 24 (13%) |
| Profession | ||
| None | 16 (5%) | 13 (7%) |
| Non-healthcare job | 262 (88%) | 154 (84%) |
| Healthcare job | 5 (2%) | 5 (3%) |
| Missing | 16 (5%) | 12 (7%) |
| Level of education | ||
| None or primary education | 45 (15%) | 27 (15%) |
| Secondary or high school education | 120 (40%) | 77 (42%) |
| Higher or university education | 119 (40%) | 68 (37%) |
| Missing | 15 (5%) | 12 (7%) |
| Source reported HIV status at baseline | ||
| Unknown | 191 (64%) | 162 (88%) |
| Positive | 25 (8%) | 22 (12%) |
| Negative | 83 (28%) | 0 (0%) |
3.3. Time-to-consultation, Patient Status and Causes of Exposure: The Median Time-to-Consultation for Non-occupational PEP (nPEP) was 19 Hours (IQR: 12.4-25.0) (Table 2).
The HIV status of the source was unknown in 64% (191/299) of cases and was described as positive for 8% (25/299) of cases. For these persons, nPEP consisted of either fixed dose combination of zidovudine (ZDV) 300 mg and lamivudine (3TC) 150 mg twice daily, or a fixed-dose combination Tenofovir (TDF) 600 mg and Lamivudine (3TC) 300 mg once daily plus a fixed dose of either Lopinavir (LPV) 400 mg and Ritonavir (RTV) 100 mg twice a day or Atazanavir (ATV) 300 mg and Ritonavir (RTV) 100 mg once a day. For 28% (83/299) of persons consulting for nPEP, the source persons were determined to have a negative HIV serology and therefore were not given PEP thus avoiding need for PEP (Table 2).
HIV testing of persons who consulted for PEP permitted identification of 4 out of 299 (1.3%) to be infected with HIV and who were started on treatment (Figure 2).
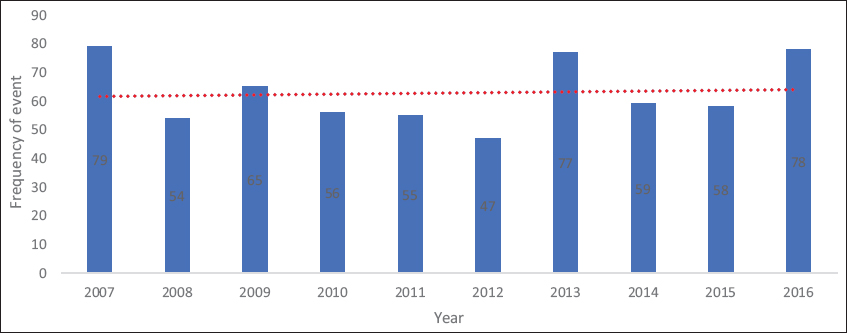
- Ten-year evolution in number of consultation for HIV post-exposure prophylaxis
With regards to the causes of accidental exposure, the most-frequent indications for consulting were: sexual assault 75% (224/299), condom slippage or breakage 10% (30/299) and unprotected consensual sexual intercourse 15% (45/299).
4. Discussion
This study described the profile of persons who consulted for PEP following exposure to HIV. The results of our study showed that over the time and generally the trend in persons seeking PEP services was relatively constant, with more males seeking services than females; the median age was 28 years with the adult group (25-49 years) most implicated. Overall, patients, on average, sought PEP services earlier than the recommended time of 72 hours with healthcare workers constituting more than half. More than two-third of those seeking PEP services had at least secondary school level education, antiretrovirals (ARV) were not prescribed for PEP in a little above a third of those who sought PEP services because the source persons were determined to be negative for HIV.
Current U.S. Centers for Disease Control and Prevention (CDC) guidelines recommend the prescription of nPEP in cases of exposure to a known HIV-infected source.1 To answer our study objectives, we specifically looked at the profile of persons seeking nPEP services in YCH.
Our analysis of gender showed that females sought nPEP services more than males. This result is unlike the studies in most Western countries where PEP is mostly sought by men, as well as men who have sex with men (MSM)2,3 and in Lausanne, Switzerland, where subjects were predominantly male (64%). This could be explained by the observation that the study in Lausanne, Switzerland, concerned PEP in general which was a similar to our general result which showed that more men than females sought PEP services. In addition, there is evidence that points to the poor health services seeking tendency among MSM in Africa4 unlike in Lausanne, Switzerland, which may have contributed to the difference when we looked specifically at nPEP
With regards to age, the median age for those with non-occupational exposure of HIV who received PEP in the study was 19 years. A population far younger than the 30 years median age found in Seattle, Washington.6 However, the age group of 25-49 years has the highest percentage of those who sought PEP. This could be related to the HIV prevalence of this age group in Cameroon which shows an increase according to statistics provided in 2011 by the Demographic and Health Survey Multiple Indicator Cluster Survey (DHS-MICS).7 Looking at the young age for nPEP, the observation that more females were seeking nPEP services and the most important cause was sexual assault, led us to believe that trans-generational sex and gender based violence may be the underlying reasons. Further research is needed to understand the underlying causes.
Regarding time to consultation, the median time for consultation was 19 hours for this study. This is close to the 17 hours in Lausanne, Switzerland3 but better than the 30 hours recorded in New South Wales, Australia, one year after the introduction of PEP guidelines,3 and 33 hours reported in San Francisco, California.8 This time frame falls in the recommended time for the initiation of PEP of within 72 hours after exposure as recommended. Exploring cause of exposure, sexual exposure appears to be the dominant reason for which individuals seek PEP. In San Francisco, U.S.A, a study reported that 93.5% of participants sought PEP because of sexual exposure.6 This is similar to the findings from another U.S. study in Seattle, Washington.6
In analyzing the HIV serology status of individuals in our study, we found that the HIV status of the source partner influenced the individual’s search for PEP. Majority of the source partners’ status were unknown as seen in other studies.6,8 However, the use of PEP against HIV infection following sexual exposure does not lead to increases in high-risk behavior.9 Determining the HIV status of the source individual is important in preventing unnecessary prescriptions for nPEP. In the case of this study, 28% (83/299) unnecessary prescriptions were avoided by determining that the source person had negative HIV status. From an epidemiological perspective offering nPEP services could help in new HIV cases identification and this is important if HIV epidemic control is to be achieved. Our results show that 1.3% (4/299) of those who consulted for nPEP tested positive for HIV and were started on ART.
5. Conclusion and Global Health Implications
Consultation for nPEP are as frequent as those occupational PEP (48% vs 52% in this study) in clinical practice at YCH. A good history of the source is important as it prevents unnecessary prescriptions of ART (which themselves have potential side effects) for persons consulting for potential HIV non-occupational exposure. In addition, adolescent or young females consulting for nPEP in clinics could be potential victims of sexual assault or gender based violence and this should be considered in clinical practice. New case identification could be bolstered by proposing “contact(s) tracing” services to those who test positive for HIV or those who seroconvert by the end of follow-up nPEP. Contact(s) tracing or partner(s) notification services have been shown to carry low risk of social harm. Young adults and adolescents and especially females consulted for nPEP and for reasons related to sexual exposure, demonstrating the need to make educate and make available PEP services accessible and friendly to young people in particular and to the population in general. Overall, many one of the important aspects in attaining HIV epidemic control is preventing new infections. PEP is one important means of doing so especially in persons who have been exposed to HIV. Therefore, it is important for the population to be aware of such services and for PEP services to be readily accessible.
Acknowledgements:
We are grateful to the Yaounde Central Hospital for granting us access to their data
Competing interests: The authors declare that they have no competing interest.
Funding: There was no funding for this study
Ethics approval: Ethical approval for the study was obtained from the Ethics Committee of Yaoundé Central Hospital (reference N° 2016/0431/CE/D/HCY). Administrative clearance was obtained from the hospital authorities and the head of service of HIV/AIDS Care and Treatment Center. Patient consent was waived for the study because it was a non-interventional study involving retrospective review of records only. However, confidentiality was respected in treating patients’ records. No data that could make identification of patients was collected
References
- Announcement:Updated Guidelines for Antiretroviral Postexposure Prophylaxis after Sexual, Injection-Drug Use, or Other Nonoccupational Exposure to HIV- United States, 2016. MMWR Morbidity and Mortality Weekly Report. 2016;65(17):458. doi:10.15585/mmwr.mm6517a5
- [Google Scholar]
- Post-exposure prophylaxis after occupational and non-occupational exposures to HIV:An overview of the policies implemented in 27 European countries. AIDS Care. 2000;12(6):695-701. doi:10.1080/09540120020014228
- [Google Scholar]
- Nonoccupational HIV post-exposure prophylaxis:a 10-year retrospective analysis. HIV Medicine. 2010;11(9):584-592. doi:10.1111/j.1468-1293.2010.00826.x
- [Google Scholar]
- Knowledge, Attitudes and Beliefs regarding Post Exposure Prophylaxis among South African Men who have Sex with Men. AIDS and Behavior. 2016;20(S3):350-356. doi:10.1007/s10461-016-1520-9
- [Google Scholar]
- The population of the regions of Cameroon according to census results and official projections. Available from https://www.citypopulation.de/Cameroon-Cities.html
- Non-Occupational Post-Exposure Prophylaxis for HIV:10-Year Retrospective Analysis in Seattle, Washington. PLoS ONE. 2014;9(8) doi:10.1371/journal.pone.0105030
- [Google Scholar]
- The 2011 Cameroon Demographic and Health Survey and multiple indicators cluster Survey Yaounde. Yaounde, Cameroun: L'Institut National de la Statistique (INS); Available from https://dhsprogram.com/pubs/pdf/HF42/HF42.pdf
- Feasibility of Postexposure Prophylaxis (PEP) against Human Immunodeficiency Virus Infection after Sexual or Injection Drug Use Exposure:The San Francisco PEP Study. The Journal of Infectious Diseases. 2001;183(5):707-714. doi:10.1086/318829
- [Google Scholar]
- Use of postexposure prophylaxis against HIV infection following sexual exposure does not lead to increases in high-risk behavior. Aids. 2004;18(5):787-792. doi:10.1097/00002030-200403260-00010
- [Google Scholar]





