Translate this page into:
Maternal Socio-Demographic Factors and Mother-to-Child Transmission of HIV in the North Region of Cameroon
* Corresponding author email: nkenfou@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
Socio-demographic factors are important risk factors for HIV infection. Maternal socio-demographic factors associated with HIV transmission from mother to child are not well elucidated to our knowledge. This study aimed to assess the maternal socio-demographic factors associated with HIV vertical transmission.
Methods:
A matched case-control study was conducted among children under 15 years of age born to HIV-infected mothers; using a structured questionnaire. The study was conducted in four health facilities in the North Region of Cameroon from July 2015 to October 2016. HIV- infected children were the cases, and HIV-uninfected children were the controls. One case was matched to nearly 4 controls according to age and sex. A total of 113 HIV-infected mothers of children under 15 years of age were purposively enrolled in the study. A questionnaire was administered to mothers and socio-demographic characteristics were collected. Blood samples were collected from the mother and her child for the determination or confirmation of HIV status. Univariate and multiple logistic regressions were used to assess associations between socio-demographic variables and HIV transmission from mother to child.
Results:
A total of 113 HIV-infected mothers and 113 children under 15 years of age were enrolled in this study. The majority of the mothers were between the age ranges of 25 years to 34 years. Of the 113 HIV-infected mothers, 69 (61%) were Muslims, 33 (32.1%) were not educated, 88 (77.8%) were unemployed, 80 (70.9%) were married, out of which 49 (61.6%) were engaged in a monogamous union. Of the 113 children (49.6%) were female, 25 (22.1%) were HIV-infected and 88 (77.9%) were HIV-exposed uninfected. At the univariate level, mothers who achieved a primary level of education were less likely to transmit HIV to infants compared to uneducated mothers [OR=0.28; CI (0.08-0.95); p=0.04]; and widows had a higher likelihood of HIV transmission to infants compared to married mothers [OR=4.65; CI (1.26-17.20); p=0.02]. Using multiple logistic regression, the maternal primary education level [aOR=0.32; CI (0.08-0.90); p=0.03] and widowerhood [aOR=7.05; CI (1.49-33.24); p=0.01] remained highly associated with the likelihood of HIV transmission to infants.
Conclusion and Global Health Implications:
Uneducated mothers and widows had a higher likelihood of mother-to-child transmission of HIV. Our findings should prompt reinforcement of prevention strategies targeting uneducated women and widows.
Keywords
HIV
Socio-demographic Factors
Mother-to-Child Transmission
North Region
Cameroon
1. Introduction
HIV Mother-To-Child Transmission (MTCT) is the passing of Human Immune deficiency Virus (HIV) from an HIV-infected mother to her baby during pregnancy, childbirth, or breastfeeding. MTCT remains the primary mode of infection in children.1 In resource-limited countries, a higher percentage of HIV-infected children (70-80%) acquire the virus during intrapartum.2 Intrauterine infection accounts for 20-30% and breastfeeding is responsible for about 40% of infections.3 Today, developed countries have reduced the rate of transmission to babies to less than 1% by a combination of interventions through the use of antiretroviral therapy for HIV-infected mothers, cesarean delivery, and formula feeding for the child. However, in most African countries, the rate remains above 10%.4
At the end of 2020, an estimated 38.4 million adults and children were living with HIV of whom 1.7 million were children under 15 years old.5 Africa is the most affected continent with 25.7 million people infected in this region, and in sub-Saharan Africa, more than 90% of HIV infection in children under 15 years of age is acquired from the mother.6 In West and Central Africa (WCA), Cameroon is the second country after Nigeria with the highest burden of the HIV epidemic.7 Six out of 25 countries in the West and Central Africa region account for 83% of people living with HIV in the region, with Nigeria accounting for 52%, Cameroon for 10%, Ivory Coast at 7%, Democratic Republic of Congo (DRC) for 7%, Ghana for 4% and Chad for 3%.7 The HIV prevalence in the population aged 15 to 49 years is 3.4% in Cameroon.8 In 2017, despite the low prevalence of HIV in adults in North Cameroon (1.6%), this region of the country was the second presenting highest positivity rate by Polymerase Chain Reaction of HIV infection among children compared to the national average (7.8% >5%).8 Pediatric acquisition of HIV remains a major challenge, and vertical transmission is responsible for 5% of total new infections occurring annually in Cameroon.9,10
Prevention of Mother-To-Child Transmission (PMTCT) programs have been identified as the most effective strategy to decrease the vertical transmission of HIV.11 Making PMTCT services accessible is essential for the elimination of infant HIV transmission in sub-Saharan Africa. However, a study has shown that PMTCT services have poor coverage and are not easily accessible to all pregnant women.12 Another study has also shown that social-demographic factors and health system factors influence the accessibility and uptake of HIV services in PMTCT.13 The socio-demographic factors include maternal age, sex of infants, infant age at testing, educational level, religion, occupation, marital status,14,15 residence,3,6 and ethnic group.16
Previous studies in Cameroon and elsewhere have identified several factors that are commonly associated with increased risk of HIV MTCT. These include viral, maternal, obstetrical, fetal, infant, socio-cultural, socio-economic11-20 and socio-demographic factors.3,6,21,22 However, the relative contribution of these factors varies between locations and can also vary over time as the epidemic matures and prevention efforts intensify. Most studies on socio-demographic factors and HIV infection have been carried out in adults. A study among young people in Tanzania found that education level, marital status, and mobility were associated with HIV infection in adults.16 Another study in India revealed that in women, the most important risk factor is being a widow while in men, the age between 25 and 45 years and low education level were found to be associated with HIV infection.14 In Cameroon, women who were married or living with their partner were less likely to be infected than single women.23
Maternal socio-demographic factors associated with HIV acquisition in children are not well elucidated to our knowledge. The Northern regions of Cameroon bear the highest illiteracy rate among other regions. Children are sometimes confined to fieldwork and pastoral activities. Thousands of girls are still not allowed to go to school. Many of them are sometimes forced into early marriage at adolescent age. Given this specific ethnocultural context, social and demographic factors may impact HIV transmission in children in the North Region of Cameroon. The goal of this study was to determine the maternal socio-demographic factors associated with HIV transmission from mother to child in the North Region of Cameroon. We hypothesized that maternal socio-demographic factors increase the rate of HIV transmission from the infected mother to her child.
2. Methods
This was a case-control study carried out in four health facilities (Garoua Regional Hospital, District Hospitals of Guider, Figuil, and Lagdo) in the North Region of Cameroon. These facilities were selected based on their high transmission rate of HIV from the mother to the child and their geographical accessibility.
The study population was children under 15 years born to HIV-infected mothers.
To obtain a statistically significant sample size of the studied population, the formula below was used.24
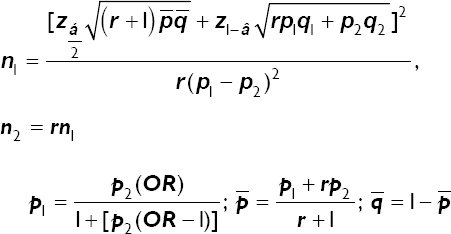
Where,
n1 Number of cases
n2 Number of controls
 z-score for two-tailed test based on α level
z-score for two-tailed test based on α level
Z1−β z-score for one-tailed test based on β level
r Ratio of controls : cases
p1 Proportion of cases with exposure
q1 1 − p1
p2 Proportion of controls with exposure
q2 1 − p2
Thus, for a power 1− β=80% =, a significant level of α = 5% , a ratio r = 3.5 , and a proportion of controls with exposure = 26%; the minimum sample size for the cases of this case-control study was 25. Because n2 = 3.5n1 , we anticipate having 85 controls. Thus, the total minimum sample size was 110.
A total of 351 children were enrolled among which 27 were HIV-infected and 324 HIV-exposed non-infected. Two (2) HIV-infected children and seventeen (17) HIV-exposed non-infected children were excluded for non-conformity. Twenty-five (25) HIV-infected children were used as cases. Each case was matched to nearly 4 HIV-exposed non-infected (control) children. Eighty-eight (88) controls were finally selected for the study. Overall 113 children (25 HIV-infected, 88 HIV-exposed non-infected) were retained for the study with their mothers (113) all HIV-infected.
2.1. Study Variables
In the current study, the dependent variable was HIV transmission from mother to child and the independent variables included age, type of religion, education level, marital status, type of union, and employment. HIV-infected mother and child pairs of the North Region of Cameroon were purposively recruited from health facilities providing services for PMTCT. A pretested questionnaire comprising fifteen (15) questions was administered in French or the local language with the assistance of a translator. From mothers, the following information was collected: age, religion, education, marital status, type of union, and employment. In children, only the age and sex were collected.
2.2. Laboratory Analysis
Blood samples were also collected from all respondents for the determination or confirmation of HIV status. HIV testing in mothers and children aged 18 months and above was performed according to the national serial algorithm for HIV rapid testing. The first test was Determine HIV1/2 (Alere Medical Co., Ltd. 357 Matsuhidai, Matsudo-shi, Chiba, Japan) and the second was OraQuick (OraSure Technologies, Inc. Bethlehem, Palestine) which is used as the confirmatory test. Oraquick HIV 1/2 is a visually read immunochromatographic test for which the test sample is introduced into the Developer Solution. A total of 50 μL of plasma was pipetted and introduced into the Developer Solution. The padded end of the device was inserted into the solution. The result was read after 20 minutes. The test was non-reactive if a line appeared only in the Control Zone, suggesting the absence of antibodies in the specimen. The appearance of two lines in both the Patient and Control zones revealed reactive results, suggesting the presence of anti-HIV antibodies in the specimen. The result was invalid if no line appeared in the Control Zone, and the test was repeated. For children less than 18 months, their virological status was determined by the Abbott qualitative Real-Time PCR Test (Abbott™ mSample Preparation System DNA Promega Corporation, Madison WI 53711USA). A dried blood spot was prepared by spotting whole blood onto a minimum of 2 circles (12 mm) on a Whatman 903 filter paper card. The test includes three major steps which are: Pre-extraction, automated nucleic acid extraction on the Abbott m2000sp (Abbott m2000 sample processing); reverse transcription and PCR amplification on the Abbott m2000rt (Abbott m2000 Real-Time). The presence of the HIV-1 target sequence is indicated by the fluorescent signal generated through the use of fluorescent-labeled oligonucleotide probes on the m2000rt instrument.25
2.3. Statistical Analysis
From the questionnaires, data were inputted into Microsoft Excel and exported into IBM-SPSS version 26 for analyses. A univariate analysis was used to examine associations between socio-demographic factors and child HIV status; Pearson’s chi-square test (Fisher exact test where relevant for two-by-two table) was used to test the relationships between qualitative variables. Associations were further quantified using the unadjusted Odds ratio (OR). Variables with p-values less than 0.05 were selected for multiple logistic regression analysis, and associations were quantified using an adjusted Odds ratio (aOR) with a 95% confidence interval (CI). The Hosmer-Lemeshow (HL test) goodness of fit test was used to assess the adequacy of the multiple logistic regression. A p-value less than 0.05 was considered statistically significant.
2.4. Ethical Approval
We obtained ethical approval from the Cameroon National Ethical Committee for Research on Human Health under the number N°2013/11/375/L/CNERH/SP. Authorization to collect and analyze samples was obtained from the Ministry of Public Health (MoPH) under the number D30-63/L/MINSANTE/SG/DROS/CRC/CEA2/DTLC. Written informed consent was obtained from the mothers as well as the assent from children when indicated.
3. Results
3.1. Socio-demographic Characteristics of Mothers
A total of 113 HIV-infected mothers have enrolled in this study as well as their children under 15 years of age. The majority of the mothers were between the age ranges of 25 years to 34 years. Of the 113 HIV-infected mothers, 69 (61%) were Muslims, 33 (32.1%) were not educated, 88 (77.8%) were unemployed, 80 (70.9%) were married, out of which 49 (61.6%) were engaged in a monogamous union. These data are presented in Table 1. Of the 113 children; 49.6% were female, 25 (22.1%) were HIV-infected and 88 (77.9%) were HIV-exposed -uninfected.
| Socio-demographic characteristics | Frequency | Percentage |
|---|---|---|
| Age | ||
| 15-19 | 6 | 5.3 |
| 20-24 | 11 | 9.7 |
| 25-34 | 63 | 55.8 |
| 35-45 | 33 | 29.2 |
| Total | 113 | 100.0 |
| Religion’ denominations | ||
| Catholic | 29 | 26.4 |
| Protestant | 11 | 10.0 |
| Muslim | 67 | 60.9 |
| Others | 3 | 2.7 |
| Total | 110 | 100.0 |
| Education | ||
| No education | 35 | 32.1 |
| Primary | 39 | 35.8 |
| Secondary or higher | 35 | 32.1 |
| Total | 109 | 100.0 |
| Marital status | ||
| Single | 4 | 3.6 |
| Living together | 8 | 7.3 |
| Divorced | 9 | 8.2 |
| Married | 78 | 70.9 |
| Widowed | 11 | 10.0 |
| Total | 110 | 100.0 |
| Type of union | ||
| Monogamy | 45 | 61.6 |
| Polygamy | 28 | 38.4 |
| Total | 73 | 100.0 |
| Employment | ||
| Not employed | 84 | 77.8 |
| Employed | 24 | 22.2 |
| Total | 108 | 100.0 |
3.2. Maternal Socio-demographic Factors Associated with HIV Transmission in Children
In univariate analysis (Table 2), maternal age, religion, type of union, and employment were not associated with HIV mother-to-child transmission. Mothers who achieved a primary level of education were less likely to transmit HIV to infants compared to uneducated mothers [OR=0.28; CI(0.08-0.95); p=0.04]; and widows had a higher likelihood of HIV transmission to infants compared to married mothers [OR=4.65; CI (1.26-17.20); p=0.02]. Since they were the only significant variables at p<0.05; they were entered into multiple logistic regression (Table 3). Maternal primary education level [aOR=0.32; CI(0.08-0.90); p=0.03] and widowerhood [aOR=7.05; CI(1.49-33.24); p=0.01] remained highly associated with the likelihood of HIV transmission to infants. Of the HIV-infected children, 40% of their mothers were uneducated, while 29.8% of the mothers of the HIV-uninfected ones were uneducated. Among HIV- infected children, 25% of their mothers were widows, as compared to 5.8% among the HIV-uninfected children (Table 2).
| HIV –(controls) N (%) | Variables | Total N (%) | Univariate OR (95%CI) | p | |
|---|---|---|---|---|---|
| Age | 0.1 | ||||
| 15-19 | 6 (6.8) | 0 (0.0) | 6 (5.3) | NA | |
| 20-24 | 7 (8.0) | 4 (16.0) | 11 (9.7) | 1.3 (0.3-5.5) | 0.7 |
| 25-34 | 52 (59.1) | 11 (44.0) | 63 (55.8) | 0.5 (0.2-1.3) | 0.1 |
| 35-45 | 23 (26.1) | 10 (40.0) | 33 (29.2) | 1 | |
| Religion | 0.9 | ||||
| Catholic | 23 (26.7) | 6 (25.0) | 29 (26.4) | 0.5 (0.04-6.8) | 0.6 |
| Protestant | 8 (9.4) | 3 (12.5) | 11 (10.0) | 0.5 (0.05-6.2) | 0.6 |
| Muslim | 53 (61.6) | 14 (58.3) | 67 (60.9) | 0.7 (0.05-11.6) | 0.8 |
| Others | 2 (2.3) | 1 (4.2) | 3 (2.7) | 1 | |
| Education | 0.04 | ||||
| No education | 25 (29.8) | 10 (40.0) | 35 (32.1) | 1 | |
| Primary | 35 (41.7) | 4 (16.0) | 39 (35.8) | 0.28 (0.08-0.95) | 0.04 |
| Secondary or higher | 24 (28.5) | 11 (44.0) | 35 (32.1) | 1.14 (041-3.18) | 0.79 |
| Marital status | 0.02 | ||||
| Single | 4 (4.7) | 0 (0.0) | 4 (3.6) | NA | |
| Co-habiting | 7 (8.1) | 1 (4.2) | 8 (7.3) | 0.55 (0.06-4.82) | 0.59 |
| Divorced | 8 (9.3) | 1 (4.1) | 9 (8.2) | 0.48 (0.06-4.16) | 0.51 |
| Married | 62 (72.1) | 16 (66.7) | 78 (70.9) | 1 | |
| Widowed | 5 (5.8) | 6 (25.0) | 11 (10.0) | 4.65 (1.26-17.20) | 0.02 |
| Type of union | 0.4 | ||||
| Monogamy | 35 (59.3) | 10 (71.4) | 45 (61.6) | 1.7 (0.5-6.1) | 0.4 |
| Polygamy | 24 (40.7) | 4 (28.6) | 28 (38.4) | 1 | |
| Employment | 0.8 | ||||
| Unemployed | 65 (77.4) | 19 (79.2) | 84 (77.8) | 1.1 (0.4-3.4) | 0.8 |
| Employed | 19 (22.6) | 5 (20.8) | 24 (22.2) | 1 | |
Legend: HIV- = HIV-exposed un-infected; HIV+ = HIV-infected; NA: Non Applicable
| Variables | Multivariate aOR (95%CI) | p |
|---|---|---|
| Education | ||
| No education | 1 | |
| Primary | 0.32 (0.08-0.90) | 0.03 |
| Secondary or higher | 1.42 (0.45-4.43) | 0.55 |
| Marital status | ||
| Single | NA | |
| Co-habiting | 0.46 (0.049-4.30) | 0.50 |
| Divorced | 0.38 (0.04-3.36) | 0.38 |
| Married | 1 | |
| Widowed | 7.05 (1.49-33.24) | 0.01 |
*Hosmer and Lemeshow Test (Chi-square=1.039; df=4; p=0.904)
4. Discussion
The present study aimed to investigate the association between maternal socio-demographic factors and HIV transmission in mother-child pairs originating from the North Region of Cameroon.
The logistic regression model showed that there was an association between the maternal education level and HIV transmission (p=0.03). Of the HIV-infected children, 40% of their mothers were uneducated, while 29.8% of the mothers of the HIV-uninfected ones were uneducated. Women with no education may be less knowledgeable of preventive measures against HIV mother-to-child transmission and this would result in poor treatment adherence. This is consistent with the findings of a case-control study in Ethiopia,6 where maternal educational level of grades 1-6 was significantly and positively associated with HIV MTCT. Moreover, mothers with a secondary level education in Ethiopia were found to be more knowledgeable about mother-to-child transmission and PMTCT, although only a very small proportion knew that elective cesarean section could be used as a method to prevent MTCT. Similar results were also reported in a study from the Northwest of Tanzania showing that education level, marital status, and mobility were associated with HIV infection in adults.16
Also, at the multivariate level, marital status was found to be associated with HIV transmission (p = 0.01) in this study. Among HIV-infected children, 25% of their mothers were widows, as compared to 5.8% among HIV-uninfected children. Generally, HIV-positive widows are left in deplorable situations. Being a widow or single parent may lead to more responsibilities, lack of emotional and economic support, and less care for oneself and also for the child, resulting in higher transmission risk. This result was consistent with a study from India, where the most important risk factor for HIV infection in women was being a widow.14 A cohort study in Rwanda also showed a statistically significant association between the HIV-1 status of infants and their mothers’ marital status.21 Other socio-demographic factors that were found to be linked to MTCT were maternal age and infants’ age at testing. The study revealed that younger mothers tend to have more HIV-infected children than older ones and, infants are more likely to be infected in the group beyond 8 weeks of age with the number of infected infants increasing from 10.3% to 22.5% at 18 months of age.22
4.1. Limitations of the Study
The study was carried out using the minimum population sample size. Only mother-child pairs who visited the hospital during the period of study were included, no enrollment was done at the community level where mobilization could be greater than in hospitals. As well, not all to whom the study was proposed have accepted to participate. Thus, included participants may not be representative of the North region of Cameroon. The questionnaire used for this study had not been used nor validated by another study.
For further studies, the population sample size needs to be increased. The study design should instead be a cohort study using a validated questionnaire. All these modifications will increase the power of the study and a more generalizable conclusion.
5. Conclusion and Global Health Implications
Uneducated mothers and widows had a higher likelihood of mother-to-child transmission of HIV. To further the elimination of mother-to-child transmission of HIV, women with no education and widows should be considered as a vulnerable target population during sensitization campaigns, thus priority should be given to them.
Acknowledgments:
Mothers who accepted to participate in this study.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no competing interests.
Financial Disclosure: Nothing to declare.
Funding/Support: No funding was received.
Ethics Approval: The study obtained approval from the Cameroon National Ethical Committee for Research on Human Health under the number N°2013/11/375/L/CNERH/SP. Permission to collect and analyze samples was granted by the Ministry of Public Health (MoPH) under the number D3063/L/MINSANTE/SG/DROS/CRC/CEA2/DTLC. The mothers provided written informed consent and assent when appropriate.
Disclaimer: None
References
- Nelson Textbook of Pediatrics. (20th ed). Philadelphia: Elsevier; 2016.
- Mother to child transmission of HIV and associated factors among HIV exposed infants at public health facilities, Dessie Town, Ethiopia. HIV AIDS (Auckl). 2019;12(11):343-350. doi:10.2147/HIV. S221409
- [Google Scholar]
- Prevention of mother-to-child transmission of HIV type 1:the role of neonatal and infant prophylaxis. Expert Rev Anti Infect Ther. 2015;13(2):169-181. doi:10.1586/147∑0.2015.999667
- [Google Scholar]
- Global Statistic:The Global HIV/AIDS Epidemic. 2020. Minority HIV AIDS Fund. https: //www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics
- [Google Scholar]
- Determinants of Mother to Child HIV Transmission (HIV MTCT);A case control study in Assela, Adama and Bishoftu Hospitals, Oromia Regional State, Ethiopia. Cell Dev Biol. 2015;4(2):1000152. doi:10.4172/2168-92961000152
- [Google Scholar]
- Out of focus:How millions of people in West and Central Africa are being left out of the global HIV response. Medecins Sans Frontieres. Published April 2016 https: //www.msf.org/sites/default/files/2016_04_hiv_report_eng.pdf
- [Google Scholar]
- Summary sheet:Preliminary findings. 2017. Cameroon Population-Based HIV-Impact Assessment CAMPHIA. CAMPHIA; https: //phia.icap.columbia.edu/wpcontent/uploads/2018/07/3471CAMPHIA_Cameroon-SS_A4_v13_requests_7.25.18.pdf
- [Google Scholar]
- 2014. Cameroon Country Operational Plan FY. PEFFAR; https: //www.state.gov/wp-content/uploads/2019/08/Cameroon-6.pdf
- Predictors of early childhood HIV testing among children of sex workers living with HIV in Cameroon. BMC Public Health. 2019;19(Suppl 1):602. doi:10.1186/s12889-019-6812-3
- [Google Scholar]
- Status of prevention of mother-to-child transmission (PMTCT) services utilization and factors affecting PMTCT service uptake by pregnant women attending antenatal care clinic in selected health facilities of Afar Regional State, Ethiopia. J Environ Public Health. 2018;2018:5127090. doi:10.1155/2018/5127090
- [Google Scholar]
- Vertical Transmission of HIV in Sub-Saharan Africa:Applying Theoretical Frameworks to Understand Social Barriers to PMTCT. Int Sch Res Notices. 2013;5 https://doi.org/10.5402/2013/420361
- [Google Scholar]
- Educational attainment as a predictor of HIV testing uptake among women of child-bearing age:Analysis of 2014 demographic and health survey in Zambia. Front Public Health. 2018;6(192) doi:10.3389/fpubh.2018.00192
- [Google Scholar]
- Socio-demographic risk factors associated with HIV infection in patients seeking medical advice in a Rural Hospital of India. J Public Health Res. 2012;1(1):79-82. doi:10.4081/jphr.2012.e14
- [Google Scholar]
- Demographic factors associated with HIV infection between low and high prevalence areas in Nigeria, 2015. Pan Afr Med J. 2019;32(Supp 1):11. doi:10.11604/pamj.supp.2019.32.1.13330
- [Google Scholar]
- HIV infection among young people in Northwest Tanzania:the role of biological, behavioural and socio-demographic risk factors. PLoS One. 2013;8(6):e66287. doi:10.1371/journal.pone.0066287
- [Google Scholar]
- Factors associated with HIV infection among children born to mothers on the prevention of mother to child transmission programme at Chitungwiza Hospital, Zimbabwe, 2008. BMC Public Health. 2013;13:1181. doi:10.1186/1471-2458-13-1181
- [Google Scholar]
- Socio-cultural factors influencing the prevention of mother-to-child transmission of HIV in Nigeria:a synthesis of the literature. BMC Public Health. 2014;14:771. doi:10.1186/1471-2458-14-771
- [Google Scholar]
- Mother-to-child transmission of HIV infection and its associated factors in Ethiopia:a systematic review and meta-analysis. BMC Infect Dis. 2018;18(1) doi:10.1186/s12879-018-3126-5
- [Google Scholar]
- Socio-structural factors influencing the prevention of mother-to-child transmission of HIV in the Democratic Republic of the Congo:A systematic review. Matern Child Health J. 2019;23(7):880-889. doi:10.1007/s10995-018-2688-6
- [Google Scholar]
- Socio-economic, clinical and biological risk factors for mother -to- child transmission of HIV-1 in Muhima health centre (Rwanda):a prospective cohort study. Arch Public Health.. 2013;71(1):4. doi:10.1186/0778-7367-71-4
- [Google Scholar]
- Maternal age, infant age, feeding options, single/multiple pregnancy, type of twin sets and mother-to-child transmission of HIV. J Trop Pediatr. 2019;65(3):280-286. doi:10.1093/tropej/fmy049
- [Google Scholar]
- Factors associated with risk of HIV-infection among pregnant women in Cameroon:Evidence from the 2016 national sentinel surveillance survey of HIV and syphilis. PLoS One. 2019;14(4):e0208963. doi:10.1371/journal.pone.0208963
- [Google Scholar]
- A novel realtime HIV-1 qualitative assay for the detection of HIV-1 nucleic acids in dried blood spots and plasma. J Virol Methods. 2011;178(1-2):216-224. doi:10.1016/j.jviromet.2011.09.015
- [Google Scholar]
- Medical Biostatistics (4th ed). Chapman &Hall/CRC Press; 2017.





