Translate this page into:
National Trends in Hospitalization, Surgical Resection, and Comorbidities in Pediatric Inflammatory Bowel Disease in the United States, 2002-2015
*Corresponding author email: deepa.dongarwar@bcm.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
Therapeutic options for pediatric inflammatory bowel disease (PIBD) have dramatically changed over the last 20 years. However, the impact of modern medical management on PIBD outcomes remains unclear. We aimed to fill this gap in the literature by using a large, validated, national database, to study the change in hospitalization rates, surgical rates, and postoperative complications in PIBD over the last decade.
Methods:
The National Inpatient Sample (NIS) Database and ICD-9-CM codes were utilized to identify inpatient admissions with a primary or secondary diagnosis of pediatric Crohn’s disease (CD) or ulcerative colitis (UC) from 2002-2015. Trends in hospitalizations, comorbidities (including malnutrition and weight loss), surgical procedures, and postoperative complications were examined using joinpoint regression analysis, a statistical modeling approach to evaluate the extent to which the rate of a condition changes over time.
Results:
There were 119,282 admissions for PIBD during the study period. The annual incidence of hospitalization increased significantly over time for both CD (average annual percent change [AAPC] 6.0%) and UC (AAPC 7.2%). The rate of intestinal resection decreased in CD patients (AAPC -6.4%) while postoperative complications remained unchanged. However, comorbidities increased significantly in CD patients (AAPC 6.8%). For pediatric UC patients, postoperative complications (AAPC 6.7%), and comorbidities (AAPC 10.2%) increased significantly over time while intestinal resection rates remained stable. Intestinal resection rate in pediatric CD has decreased over time, but not in pediatric UC.
Conclusion and Global Health Implications:
Annual incidence of hospitalization and comorbidities continue to increase in PIBD. Intestinal resection rate in pediatric CD has decreased over time, but not in pediatric UC. Our findings emphasize the critical need for prevention and novel therapeutic options for this vulnerable patient population.
Keywords
Pediatric
Inflammatory Bowel Disease
Crohn’s Disease
Ulcerative Colitis
National Trends
HCUP NIS
1. Introduction
Inflammatory bowel diseases (IBD) are chronic, relapsing and remitting gastrointestinal diseases that require lifelong medical treatment, intermittent hospitalization, and need for surgical intervention in a proportion of patients.1 The ultimate goal of medical treatment is to achieve remission, with the least amount of side effects possible. The landscape of therapeutic options for IBD has dramatically changed since the early 2000s with the widespread use of biologic medications for Crohn’s disease (CD) and ulcerative colitis (UC).2 Similarly, surgical techniques3 and peri- and postoperative management of patients4,5 have evolved.
The ultimate impact of these advancing treatment options on outcomes in PIBD remains unclear. There have been multiple studies looking at IBD in adults 6–10 but pediatric data is very limited. Park et al. determined that hospital utilization has decreased, but this was not associated with a decreased risk of surgery.11 Another study found a nationwide increase in the annual incidence of hospitalization for pediatric CD and UC over a 12 year period, however, intestinal resection rates only increased in pediatric CD.12 The impact of evolving treatment options on surgical complication rates in IBD is similarly controversial. Studies comparing children with IBD treated with biologic versus non-biologic therapy prior to bowel resection did not find an increased risk of postoperative complications in children receiving biologics.13–15 However, multiple studies in adult patients have found conflicting results.16–22
As medical and surgical management continue to progress, the overall nationwide impact on hospitalization, surgical rates, and postoperative complications in PIBD remains unclear. We aimed to fill this gap in the literature by examining the change in these indices (hospitalizations, surgical rates, and postoperative complications) over the last decade. We hypothesized that hospitalization rates, surgical rates, and postoperative complications in pediatric PIBD have decreased over time.
2. Methods
This is a retrospective study using the Nationwide Inpatient Sample (NIS), which is developed for the Healthcare Cost and Utilization Project (HCUP) and sponsored by the Agency for Healthcare Research and Quality (AHRQ).23 It is the largest all-payer publicly available data that contains information regarding more than 7 million unweighted and 35 million weighted samples of inpatient hospitalizations among all non-federal and non-rehabilitation hospitals in the United States. It contains patient socio-demographics, diagnoses, procedures, and hospital characteristics information, which is obtained from the discharge records of each hospital stay.
The NIS used the International Classification of Diseases, Ninth Edition, Clinical Modification codes (ICD-9 CM) to document the diagnoses and procedures associated with each hospital stay. Starting in the last quarter of 2015, NIS implemented ICD-10 CM, therefore we limited the data to the third quarter of 2015. All encounter data in the NIS are presented per visit or per admission and not per patient, with an effort to protect patient confidentiality and it does not contain any identifiers that would make it possible to link various encounters for the same patient over time.
2.1. Study Sample
Between January 1, 2002 and September 30, 2015, among patients less than 18 years of age, we identified patients with primary or secondary diagnosis of CD and ulcerative colitis. For Crohn’s disease, we used ICD-9 codes 555.0 (Crohn’s disease of small intestine without complications), 555.1 (Crohn’s disease of large intestine without complications), 555.2 (Crohn’s disease of both small and large intestine without complications), or 555.9 (Crohn’s disease, unspecified, without complications). For UC we used ICD-9 codes 556.0–556.9, which includes ulcerative (chronic) enterocolitis, ulcerative (chronic) ileocolitis, ulcerative proctitis, ulcerative (chronic) rectosigmoiditis without complications, left-sided ulcerative (chronic) colitis, ulcerative (chronic) pancolitis without complications, other ulcerative colitis, and ulcerative colitis, unspecified. As CD and UC are not typically diagnosed among infants less than a month of age, we excluded all birth hospitalizations and patients less than one month of age. Similarly, we excluded discharges in which the entire hospitalization, from admission to discharge, was completed before the end of the first month of life. Among the patients with a diagnosis of CD or UC (exposure), we calculated the rates of comorbidities, surgical procedures and postoperative complications (outcomes), which were also coded in ICD-9 format in the data. Specific comorbidities included obesity (278.01[morbid obesity], 278.02 [overweight]), failure to thrive (783.41 [Failure to thrive], 783.7 [adult failure to thrive]), nutritional deficiency (260 [kwashiorkor], 261 [nutritional marasmus], 262 [other severe protein-calorie malnutrition], 263 [malnutrition of moderate degree]), abnormal weight loss (783.2 group) and anorexia (783.0). Surgical procedures included in this study were excision of the small intestine (456 group), open and other partial excision of the large intestine (457 group), total intra-abdominal colectomy (458 group), laparoscopic partial excision of the large intestine (173 group), pull through resection of rectum (484 group), abdominoperineal resection of rectum (485 group), and other resection of rectum (486 group). Postoperative complications include anastomotic leak (9974 group), urinary tract infection (9975), wound infection (9983 group), and other postoperative infections (9985 group).
The covariates included in the study were patients’ socio-demographic and hospital stay characteristics such as age, ethnicity (non-Hispanic vs. Hispanic) and race (White, Black and Others), zip income quartile, primary payer and disposition.
Descriptive statistics including frequencies and proportions describing the socio-demographic and hospital stay characteristics were included among those diagnosed with CD and UC. Furthermore, frequencies and proportions of different types of comorbidities, surgical procedures and postoperative complications were calculated for those with CD and UC. Next, we calculated the temporal trends in the prevalence of CD and UC per 10,000 hospitalizations, and trends in the rates of comorbidities, surgeries and postoperative complication per 100 CD and UC hospitalizations over the years 2002 - 2015. For the purposes of calculating trends, we combined the open and other partial excision of the large intestine and the laparoscopic partial excision of the large intestine to “open, laparoscopic partial and other partial excision of the large intestine.” Similarly, we combined pull-through resection of the rectum, abdominoperineal resection of rectum, and other resection of rectum to “pull-through, abdominoperineal and other resection of rectum.” Finally, we combined urinary tract infection, wound infection, and other postoperative infections to “other postoperative infection.”
We utilized the joinpoint regression technique, a statistical modeling approach to evaluate the extent to which the rate of a condition changes over time, to assess the temporal trends.24 Overall trend for the entire time period is denoted by average annual percent change (AAPC) for each outcome of interest in the study. All tests of hypotheses were two-tailed with type-1 error rate set at 5%. All statistical analyses were performed using R (version 3·5·1), RStudio (version 1·1·423), and Joinpoint Regression Program version 4.7.0.0 (National Cancer Institute). The institutional review board of Baylor College of Medicine classified this study as exempt since it utilized publicly available and de-identified data.
3. Results
We analyzed a total of 119,282 pediatric hospitalizations involving IBD. Of these, 73,339 (61.5%) were diagnosed with CD and 45,943 (38.5%) were diagnosed with UC (Table 1). Table 1 compares selected characteristics of admitted children with CD and UC. The majority of children in both groups were over 11 years old, of non-Hispanic White race, and in a higher family income bracket.
| CD (n=73,339) | % Total 39 | UC (n=45,943) | % Total 943 | |
|---|---|---|---|---|
| Age | ||||
| 0-5 years | 2,580 | 3.52% | 3,105 | 6.76% |
| 6-10 years | 8,476 | 11.56% | 6,895 | 15.01% |
| 11-14 years | 25,314 | 34.52% | 15,046 | 32.75% |
| 15-19 years | 36,969 | 50.41% | 20,897 | 45.48% |
| Race | ||||
| NH-White | 41,962 | 57.22% | 25,518 | 55.54% |
| NH-Black | 8,793 | 11.99% | 3,795 | 8.26% |
| Hispanic | 4,692 | 6.40% | 4,875 | 10.61% |
| Others | 3,284 | 4.48% | 2,633 | 5.73% |
| Zip Income Quartile | ||||
| Lowest | 13,641 | 18.60% | 7,767 | 16.91% |
| 2nd | 15,210 | 20.74% | 10,198 | 22.20% |
| 3rd | 17,750 | 24.20% | 11,698 | 25.46% |
| Highest | 25,591 | 34.89% | 15,497 | 33.73% |
| Primary Payer | ||||
| Medicare | 105 | 0.14% | 30 | 0.07% |
| Medicaid | 18,108 | 24.69% | 11,382 | 24.77% |
| Private insurance | 50,480 | 68.83% | 31,388 | 68.32% |
| Self-pay | 1,413 | 1.93% | 833 | 1.81% |
| No charge | 65 | 0.09% | 41 | 0.09% |
| Other | 3,023 | 4.12% | 2,211 | 4.81% |
| Disposition Type | ||||
| Routine | 68,045 | 92.78% | 42,408 | 92.31% |
| Transfer to Short-term Hospital | 1,122 | 1.53% | 1,007 | 2.19% |
| Transfer other type of facility | 311 | 0.42% | 205 | 0.45% |
| Home Healthcare | 3,679 | 5.02% | 2,184 | 4.75% |
| Against medical advice (AMA) | 112 | 0.15% | 35 | 0.08% |
| Died in hospital | 31 | 0.04% | 84 | 0.18% |
| Discharged alive, destination unknown | - | 0.01% | 16 | 0.03% |
Note 1: ‘-‘ represents values less than 10, which are not to be reported as per HCUP guidelines. Note 2: Columns do not contain missing values to prevent the identification of cell values less than 10. So column totals may not match
3.1. Hospitalizations
The annual incidence of hospitalization increased significantly over time for both CD (average annual percent change [AAPC], 6.0, 95% confidence interval [CI] 4.7, 7.2) and UC (AAPC, 7.2, 95% CI 6.2, 8.1, Figure 1). The surgical resection rate decreased in CD patients (AAPC, -6.4, 95% CI, -8.7, -4.1) while postoperative complications remained unchanged (Supplemental Figure 1A). However, comorbidities increased significantly in CD patients (AAPC, 6.8, 95% CI, 4.6, 9.0). For pediatric UC patients, postoperative complications (AAPC, 6.7, 95% CI, 1.2, 12.4), and comorbidities (AAPC, 10.2, 95% CI, 8.8, 11.6) increased significantly over time while intestinal resection rates remained stable (Supplemental Figure 1B).
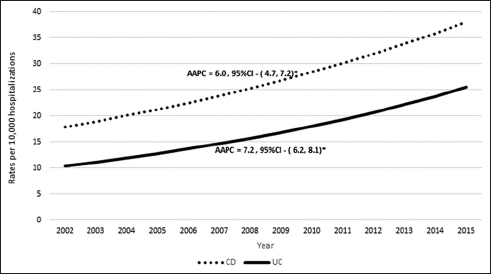
- Annual incidence of hospitalization for Crohn’s disease (CD) and ulcerative colitis (UC) from 2002-2015 AAPC= Average Annual Percent Change. *p≤0.05
3.2. Comorbidities
When specific comorbidities were analyzed separately, all comorbidities increased significantly over time in UC patients (Supplemental Figure 2B, Table 2). In CD patients, all comorbidities increased significantly over time except malnutrition (Supplemental Figure 2A). While CD patients did not have a significant increase in malnutrition overall, there was a visible rise in malnutrition rates from 2007-2012, followed by a decrease from 2012-2015 in this patient group.
| CD (n=73,339) | % Total 339 | UC (n=45,943) | % Total | |
|---|---|---|---|---|
| Comorbid conditions | ||||
| Obesity | 830 | 1.13% | 717 | 1.56% |
| Malnutrition - Failure to thrive | 1,759 | 2.40% | 458 | 1.00% |
| Nutritional deficiency | 5,315 | 7.25% | 2,318 | 5.05% |
| Abnormal Weight loss | 5,016 | 6.84% | 2,568 | 5.59% |
| Anorexia | 838 | 1.14% | 476 | 1.04% |
| Surgeries | ||||
| Excision of small intestine | 1,818 | 2.48% | 515 | 1.12% |
| Open and other partial excision of the large intestine | 4,411 | 6.01% | 704 | 1.53% |
| Total intra-abdominal colectomy | 368 | 0.50% | 2,880 | 6.27% |
| Laparoscopic partial excision of the large intestine | 4,288 | 5.85% | 721 | 1.57% |
| Pull-through resection of rectum | 20 | 0.03% | 891 | 1.94% |
| Abdominoperineal resection of rectum | 43 | 0.06% | 545 | 1.19% |
| Other resection of rectum | 126 | 0.17% | 1,388 | 3.02% |
| Postoperative complications | ||||
| Anastomotic leak | 730 | 1.00% | 631 | 1.37% |
| Urinary tract infection | 49 | 0.07% | 30 | 0.07% |
| Wound infection | 95 | 0.13% | 85 | 0.19% |
| Other postoperative infection | 613 | 0.84% | 391 | 0.85% |
3.3. Surgeries and Postoperative Complications
Changes in the rates of specific surgical operations and postoperative complications were also analyzed (Table 2). For both CD and UC patients, the rate of open, laparoscopic and other partial excision of the large intestine decreased significantly over time (Supplemental Figure 3), while other operations did not change. The rate of anastomotic leak decreased for CD (Supplemental Figure 4A) and increased for UC patients (Supplemental Figure 4B), however, these trends did not reach statistical significance. Other postoperative infection rates increased significantly over time for both CD and UC patients (Supplemental Figure 4). Also, there was a significant increase in age at the time of surgery in UC patients over the study period (Supplemental Figure 5), while this change was not observed in CD patients.
4. Discussion
We utilized a large, national, inpatient database to assess changes in hospitalization rates, comorbidities, surgical rates, and postoperative complications in PIBD over a 13-year period. The study period included major advancements in the medical and surgical management of PIBD patients. Despite evolving therapeutic options, we found that the annual incidence of hospitalization for PIBD patients has increased over time. This is in agreement with multiple studies which have similarly documented increasing hospitalizations in PIBD.12,25–28 However, some studies have reported stable or decreasing incidence of IBD in North America.29,30 It is clear from these conflicting data, that overall trends in incidence and prevalence of IBD in the United States are not clearly established. Interestingly, hospitalized PIBD patients originated from higher-income ZIP codes. This finding is in agreement with another study where PIBD incidence by ZIP code significantly correlated with family income.31
While the surgical resection rate has decreased in CD patients, it remains unchanged in pediatric UC. This may demonstrate that the evolving medical management options for PIBD have been more effective at mitigating intestinal resection risk in patients with pediatric CD than UC. Alternatively, this could reflect an overall hesitancy to perform surgery in CD compared with UC, as surgery can be considered “curative” in the UC patient. Of note, the main driver of this decreasing surgical rate in CD in our study was the significant decrease in partial excision of the large intestine. While a similar decrease in partial excision of the large intestine is noted in UC patients, this was balanced by a trend toward an increase in the rate of other intra-abdominal surgeries, though these did not separately reach statistical significance.
Postoperative complications in our study increased in pediatric UC patients over time. While some studies suggest that preoperative biologic use can increase the risk of postoperative complications in adults,16,18 there have been a number of observations to suggest that biologic use does not increase the risk of postoperative complications in PIBD.13–15 Therefore, it is possible that patient factors, such as the severity of disease at the time of surgery, may be the cause of complications rather than the use of these newer medical therapies. However, it is conceivable that the patient’s surgery may be delayed, as there are more available therapeutic options that can be used prior to surgery. If the disease continues to progress throughout these medication trials, it is possible that the disease is at a more severe stage at the time of surgery, leading to an increased risk of complications. Due to limitations of data provided through the NIS we were unable to assess medications used throughout the course of each patient’s disease. However, this theory is supported by the fact that the average age at the time of surgery increased significantly in UC patients over time in our study (Supplemental Figure 5). Interestingly, we did not see a change in postoperative complication rate or average age at surgery in the pediatric CD population.
Rates of comorbidities increased in both pediatric CD and UC. The leading comorbidities in these patients were nutrition-related, including malnutrition and abnormal weight loss. While improvement in nutritional status is one of the major facets of PIBD care, this finding implies that overall nutritional status in PIBD patients with high disease activity (i.e. requiring hospitalization) has not been improving over time. Patients with active disease are more likely to be undernourished,32 therefore it is possible that increasing malnutrition is a surrogate marker for worsening overall disease status and/or medical treatment failure in these patients.
Interestingly, there was also an increase in rates of obesity in both CD and UC patients. Obesity is a significant public health threat, which can also affect patients with PIBD. A study found that 23.6% of pediatric CD patients and 30.1% of pediatric UC patients are overweight or obese, rates that are comparable to the general population. 33,34 While it is likely that the increase in obesity that we observed was congruent with the increasing prevalence of overweight and obesity in pediatric patients across the country, it remains important to specifically monitor for this comorbidity in PIBD patients.
There are certain limitations inherent to this study. Any study relying on database analysis runs the risk of misclassification of documented diagnoses and procedure variables, and cannot take into account differential reporting of diagnoses over time (such as the comorbidities examined in this study). Also, in the NIS the unit of observation is a hospitalization as opposed to a unique patient (as specific patient identifiers are removed). Therefore, if the same patient was hospitalized multiple times, it was counted as multiple unique hospitalizations. The most significant limitation is the lack of specific clinical details, including information about the severity of disease and medical management. Regardless of these limitations, the NIS is a large, validated, population-based dataset representative of all hospitalizations in the United States, which enhances the generalizability of our findings.
5. Conclusions and Global Health Implications
In conclusion, our study represents a substantial body of data evaluating changes in PIBD outcomes, including hospitalizations, comorbidities, surgical rates, and postoperative complications over time. Contrary to our hypothesis, the annual incidence of hospitalization and comorbidities increased in these patients despite the increasing medical and surgical care options. Future studies are needed to evaluate the factors contributing to increased hospitalization and comorbidities in these patients, as well as possible preventative measures in order to decrease the burden of PIBD.
Acknowledgments:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no competing interests.
Financial Disclosure: Nothing to declare.
Funding/Support: This work was supported by the Health Resources and Services Administration (HRSA) [grant number 1 D34HP31024-01-00] for the project titled Baylor College of Medicine (BCM) Center of Excellence in Health Equity, Training & Research. This work was also supported by philanthropy from the Gutsy Kids Fund: by the Karen and Brock Wagner family; and by the Klaasmeyer family [to R.K.]. These funding bodies played no role in the design of the study, the collection, analysis and interpretation of data, or writing of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of BCM, HRSA, or the Agency for Healthcare Research and Quality.
Ethics Approval: The institutional review board of Baylor College of Medicine classified this study as exempt since it utilized publicly available and de-identified data.
Disclaimer: None.
References
- Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12(4):205-217. doi:10.1038/nrgastro.2015.34
- [Google Scholar]
- Biologic agents for IBD:Practical insights. Nat Rev Gastroenterol Hepatol. 2015;12(9):537-545. doi:10.1038/nrgastro.2015.135
- [Google Scholar]
- Advances in the surgical management of inflammatory bowel disease. Curr Opin Gastroenterol. 2012;28(1):47-51. doi:10.1097/MOG.0b013e32834d8fcb
- [Google Scholar]
- Perioperative management of ileocecal Crohn's disease in the current era. Expert Rev Gastroenterol Hepatol. 2020;14(9):843-855. doi:10.1080/17474124.2020.180224
- [Google Scholar]
- Therapy for Crohn's disease:A review of recent developments. Curr Gastroenterol Rep. 2018;20(5):19. doi:10.1007/s11894-018-0625-x
- [Google Scholar]
- Inflammatory bowel disease in the United States from 1998 to 2005:Has infliximab affected surgical rates? Am Surg. 2009;75(10):976-980.
- [Google Scholar]
- Infliximab reduces hospitalizations and surgery interventions in patients with inflammatory bowel disease:A systematic review and meta-analysis. Inflamm Bowel Dis. 2013;19(10):2098-2110. doi:10.1097/MIB.0b013e31829936c2
- [Google Scholar]
- Decreasing colectomy rate for ulcerative colitis in the United States between 2007 and 2016:A time trend analysis. Inflamm Bowel Dis. 2020;26(8):1225-1231. doi:10.1093/ibd/izz247
- [Google Scholar]
- Complications and surgery in the inflammatory bowel diseases biological era. Curr Opin Gastroenterol. 2014;30(4):378-384. doi:10.1097/MOG.0000000000000078
- [Google Scholar]
- Surgical rates in the era of biological therapy:up, down or unchanged? Curr Opin Gastroenterol. 2017;33(4):246-253. doi:10.1097/MOG.0000000000000361
- [Google Scholar]
- Utilization trends of anti-TNF agents and health outcomes in adults and children with inflammatory bowel diseases:A single-center experience. Inflamm Bowel Dis. 2014;20(7):1242-1249. doi:10.1097/MIB.0000000000000061
- [Google Scholar]
- Nationwide temporal trends in incidence of hospitalization and surgical intestinal resection in pediatric inflammatory bowel diseases in the United States from 1997 to 2009. Inflamm Bowel Dis. 2013;19(11):2423-2432. doi:10.1097/MIB.0b013e3182a56148
- [Google Scholar]
- Risk factors for complications after ileocolonic resection for Crohn's disease with a major focus on the impact of preoperative immunosuppressive and biologic therapy:A retrospective international multicentre study. United European Gastroenterol J. 2016;4(6):784-793. doi:10.1177/2050640615600116
- [Google Scholar]
- The effect of biologics on post-operative complications in children with inflammatory bowel disease and bowel resection. J Pediatr Gastroenterol Nutr. 2019;68(3):334-338. doi:10.1097/MPG.0000000000002159
- [Google Scholar]
- Duration of disease may predict response to infliximab in pediatric ulcerative colitis. J Clin Gastroenterol. 2014;48(3):248-252. doi:10.1097/MCG.0b013e31829f2e06
- [Google Scholar]
- Use of infliximab within 3 months of ileocolonic resection is associated with adverse postoperative outcomes in Crohn's patients. J Gastrointest Surg. 2008;12(10):1738-1744. doi:10.1007/s11605-008-0646-0
- [Google Scholar]
- Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases:a meta-analysis. J Crohns Colitis. 2013;7(11):853-867. doi:10.1016/j.crohns.2013.01.014
- [Google Scholar]
- Effect of preoperative biologic drugs on complications and function after restorative proctocolectomy with primary ileal pouch formation:Systematic review and meta-analysis. Inflamm Bowel Dis. 2015;21(1):79-92. doi:10.1097/MIB.0000000000000232
- [Google Scholar]
- Anti-TNF-alpha therapies do not increase early postoperative complications in patients with inflammatory bowel disease. An Italian single-center experience. Int J Colorectal Dis. 2011;26(11):1435-1444. doi:10.1007/s00384-011-1236-2
- [Google Scholar]
- Meta-analysis:Effect of preoperative infliximab use on early postoperative complications in patients with ulcerative colitis undergoing abdominal surgery. Aliment Pharmacol Ther. 2012;36(10):922-928. doi:10.1111/apt.12060
- [Google Scholar]
- Complications in surgery for Crohn's disease after preoperative antitumour necrosis factor therapy. Br J Surg. 2014;101(5):539-545. doi:10.1002/bjs.9439
- [Google Scholar]
- Anti-tumor necrosis factor therapy is associated with infections after abdominal surgery in Crohn's disease patients. Am J Gastroenterol. 2013;108(4):583-593. doi:10.1038/ajg.2012.464
- [Google Scholar]
- Joinpoint Regression Program Version 4.8. 0.1 - April. In: Statistical Methodology and Applications Branch, Surveillance Research Program. National Cancer Institute; 2020.
- [Google Scholar]
- Increasing hospitalizations in inflammatory bowel disease among children in the United States, 1988-2011. Inflamm Bowel Dis. 2014;20(10):1754-1760. doi:10.1097/MIB.0000000000000195
- [Google Scholar]
- Trends in hospitalizations of children with inflammatory bowel disease within the United States from 2000 to 2009. J Investig Med. 2013;61(6):1036-1038. doi:10.2310/JIM.0b013e31829a4e25
- [Google Scholar]
- Comparative incidence of inflammatory bowel disease in different age groups in the United States. Inflamm Bowel Dis. 2019;25(12):1983-1989. doi:10.1093/ibd/izz092
- [Google Scholar]
- Prevalence of inflammatory bowel disease in pediatric and adult populations:Recent estimates from large national databases in the United States,2007-2016. Inflamm Bowel Dis. 2020;26(4):619-625. doi:10.1093/ibd/izz182
- [Google Scholar]
- Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century:A systematic review of population-based studies. Lancet. 2017;390(10114):2769-2778. doi:10.1016/S0140-6736(17)32448-0
- [Google Scholar]
- Trends in epidemiology of pediatric inflammatory bowel disease in Canada:Distributed network analysis of multiple population-based provincial health administrative databases. Am J Gastroenterol. 2017;112(7):1120-1134. doi:10.1038/ajg.2017.97
- [Google Scholar]
- Parental education may differentially impact pediatric inflammatory bowel disease phenotype risk. Inflamm Bowel Dis. 2020;26(7):1068-1076. doi:10.1093/ibd/izz225
- [Google Scholar]
- A cross-sectional study on malnutrition in inflammatory bowel disease:Is there a difference based on pediatric or adult age grouping? Inflamm Bowel Dis. 2019;25(8):1428-1441. doi:10.1093/ibd/izy403
- [Google Scholar]
- Prevalence and epidemiology of overweight and obesity in children with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17(10):2162-2168. doi:10.1002/ibd.21585
- [Google Scholar]
- Biologic agents are associated with excessive weight gain in children with inflammatory bowel disease. Dig Dis Sci. 2017;62(11):3110-3116. doi:10.1007/s10620-017-4745-1
- [Google Scholar]





