Translate this page into:
Prevalence, Epidemiological, and Clinical Profile of Patients Coinfected with Human Immunodeficiency Virus and Tuberculosis in the Coronavirus Disease 2019 Context in Health Facilities in the East Region, Cameroon

*Corresponding author: Onana Akoa François Anicet, MPH, PhD International Center for Multidisciplinary Research at the University of Lisala, Democratic Republic of Congo, Department of Public Health, Catholic University of Central Africa, Yaoundé, Cameroon. Tel: +237696121581 onanaanicet@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: François Anicet OA, Kouanfack C, Dama U, Nkfusai C, Abanda JN, Tchoffo D, et al. Prevalence, epidemiological, and clinical profile of patients coinfected with human immunodeficiency virus and tuberculosis in the coronavirus disease 2019 context in health facilities in the east region, Cameroon. Int J Matern Child Health AIDS. 2024;13:e006. doi: 10.25259/IJMA_683.
Abstract
Background and Objective
Suspected cases of tuberculosis (TB) are identified for confirmation by bacteriological tests through clinical screening for TB in people living with human immunodeficiency virus (HIV) during routine visits or when antiretrovirals (ARVs) are dispensed. Our aim is to determine the prevalence and describe the epidemiological and clinical characteristics of HIV-TB coinfected patients in the coronavirus disease 2019 (COVID-19) setting in health facilities in the East Region of Cameroon. This study addresses knowledge gaps on HIV-TB coinfection during COVID-19, aiming to provide insights into the interaction and impact of HIV, TB, and COVID-19 on individuals’ health.
Methods
This was an observational study. It involved two retrospective cohorts of HIV-TB coinfected patients before and after the COVID-19 pandemic. We conducted manual reviews of the medical records and antiretroviral therapy (ART) and TB registers of 262 patients. These patients were coinfected with HIV and TB during the period from April 2019 to April 2021 in 11 health facilities in the East Cameroon health region. The sociodemographic and clinical characteristics of the cases were extracted from the consultation registers and entered into the KoBo Collect application, then analyzed using the Statistical Package for the Social Sciences (SPSS) software, version 25.
Results
In this study of 262 HIV-TB coinfection cases, 60.3% occurred before COVID-19, and 39.7% during the pandemic. HIV-TB coinfection prevalence among HIV patients was 1%. Patients averaged 39.3 years in age, with a significant shift in sex ratios from 0.65 to 1.33 between pre-COVID-19 and COVID-19 cohorts. Education varied, with 45.8% having secondary education, 44.8% with primary, 2.4% having higher education, and 7.1% having none. Most (78.9%) had professional occupations, and 53.7% lived in rural areas. The majority were newly diagnosed (96.3% before COVID-19; 93.3% during COVID-19), with 3.7% relapses and 4.2% discontinuing treatment. Most had pulmonary TB (84.9%) and were aware of treatment duration (94.6%). About 65.4% experienced treatment-related adverse events. Regarding family support, 69.3% received help with medication. However, the concern was 80.6% did not adhere to anti-COVID-19 measures.
Conclusion and Global Health Implications
Gender was significantly associated with compliance. Most patients were on treatment, but a small percentage had discontinued it. Patients need to be made aware of the importance of complying with anti-COVID-19 barrier measures to prevent a potential worsening of the health situation. Moreover, clinical and biological monitoring needs to be stepped up throughout the course of anti-TB treatment.
Keywords
Prevalence
Coronavirus Disease 2019
Coinfection
Tuberculosis/Human Immunodeficiency Virus
Cameroon
INTRODUCTION
The human immunodeficiency virus (HIV) pandemic represents a major challenge for tuberculosis (TB) control programs worldwide.[1] Importantly, HIV/ acquired immunodeficiency syndrome (AIDS) predisposes to Mycobacterium tuberculosis (MTB) infection and increases the likelihood of newly acquired (TB) infection progressing to active disease status and increases the rate of recurrent TB. The lifetime risk of developing active TB in immunocompetent adults is estimated at 10%, but in people living with HIV (PLHIV) infected with MTB, the annual risk of developing active TB exceeds 10%.[2] In order to contribute to a 90% reduction in TB incidence and 95% reduction in mortality by 2035, the global “END TB” strategy aims to scale up efforts to expand preventive TB therapy (PTT) as a central intervention in HIV programs.[3] PLHIV are much more likely to develop active TB than HIV-negative people.[4] The use and implementation of preventive strategies have remained woefully inadequate in the fight against TB in PLHIV. TB remains a public health problem in resource-limited countries and to this day has remained a major cause of death among PLHIV infection.
In 2018, an estimated 25,000 PLHIV died from TB, accounting for a third of all HIV-related deaths and a sixth of all TB deaths. It is important to note that HIV/AIDS predisposes to infection with MTB and increases the likelihood that newly acquired TB infection will progress to active disease status and increase the rate of recurrent TB. The lifetime risk of developing active TB in immunocompetent adults is estimated at 10%, but in PLHIV infected with MTB, the annual risk of developing active TB exceeds 10%.[2] In order to contribute to a 90% reduction in TB incidence and a 95% reduction in mortality by 2035, the global END TB strategy aims to intensify efforts to scale up PTT as a central intervention in HIV programs. HIV-infected individuals are 16 times more likely to develop TB than those who are uninfected (uncertainty interval: 14–18). TB is the leading cause of death among PLHIV. TB and HIV form a deadly combination, with each accelerating the progression of the other. In the absence of appropriate treatment, an average of 45% of HIV-negative TB patients will die, as will virtually all those who are also HIV-positive.[5] In 2021, around 187,000 people died from HIV-associated TB. The percentage of notified cases of TB for which an attested HIV test result was available was only 76% in 2021, compared with 73% in 2020. The World Health Organization African Region is the most affected by HIV-associated TB. Globally, among TB patients with known HIV infection, 46% were receiving antiretroviral treatment (ART) in 2021.[6] In Cameroon, HIV infection is common among patients with active TB and disproportionately affects women.[7] The aim of our study is to[1] determine the prevalence and[2] describe the epidemiological and clinical characteristics of HIV-TB coinfected patients in the coronavirus disease 2019 (COVID-19) setting in health facilities in the East Region.
METHODS
Study Setting
For the purposes of our research, we have concentrated solely on the East region, which is one of the largest regions in the country. It is bordered to the north by Adamaoua, to the east by Central Africa Republic, to the south by the Republic of Congo, and to the west by the southern and central regions. According to the 2023 report on target populations (second edition) by the Health Information Unit (CIS) of the Ministry of Public Health, Cameroon, the population in 2023 in the East region (for both sexes) is estimated at around 1,424,519 inhabitants. The East region currently has 27 TB diagnosis and treatment centers. TB treatment is standardized and free in Cameroon. In reality, the logic of the health system is that TB patients should be distributed more or less equitably, according to their place of residence, across all 27 decentralized TB Treatment Centers. Table 1 shows the distribution of the different TB Treatment Centers in the health districts (HDs).
| # | HD | TB treatment center |
|---|---|---|
| 1 | HD Bertoua | URLTB |
| CSC Tigaza | ||
| Regional Hospital of Bertoua | ||
| Prison centrale | ||
| 2 | HD Belabo | CSC Belabo |
| 3 | HD Doume | CSC Doume |
| CMA Doumaintang | ||
| 4 | HD Abong Mbang | HD Abong Mbang |
| CSC Sague (Nguelemendouka) | ||
| 5 | HD Messamena | HD Messamena |
| 6 | HD Mbang | HD Mbang |
| 7 | HD Lomié | HD Lomié |
| CMA Messok | ||
| CMA Ngoyla | ||
| 8 | HD Batouri | PLT Batouri (Fondation Damien) |
| 9 | HD Ndelele | CSC Ndelele |
| CMA Mindourou | ||
| CMA Kentzou | ||
| 10 | HD Yokadouma | HD Yokadouma |
| CSI Gatto | ||
| 11 | HD Moloundou | HD Moloundou |
| HC Salapoumbe | ||
| 12 | HD Garoua-Boulai | CSC Garoua-Boulai |
| HP Garoua-Boulai | ||
| HD Garoua-Boulai | ||
| 13 | HD Betare-Oya | HD Kette |
| HD Betare-oya |
HD: Health district, TB: Tuberculosis, URLTB: Regional Tuberculosis Unit, CSC: Catholic Health Center, CMA: Medicalised Health Center, CSI: Integrated Health Service, PLT: Leprosy and Tuberculosis Pavilion, HC: Catholic Hospital.
In each HD of the region, we randomly selected a TB Treatment Center. We had two data collection sites, namely, the TB treatment centers and the HIV Management Units. In the TB treatment centers selected in each health district (HD), we listed in the TB register all HIV/TB coinfected patients during the periods from April to September 2019 and from May to October 2020. The questionnaire was administered to patients identified at the UPECs of randomly selected sites. The type of sampling was probabilistic (cluster sampling). We excluded all patients under the age of 18 and all those who did not wish to take part in the study.
Study Type and Study Period
This investigation adopts a retrospective cohort study design, specifically focusing on the observation and analysis of HIV/TB coinfected patients both before and after the onset of the COVID-19 pandemic. Unlike a longitudinal observational study, a retrospective cohort study involves the collection and examination of historical data related to individuals with a shared characteristic – in this case, HIV/TB coinfection – over a specified period. The study spans a comprehensive 25-month duration, ranging from April 2019 to April 2021. This extended time frame allows for a thorough examination of the dynamics and outcomes among the cohort members within the context of the evolving circumstances surrounding the COVID-19 pandemic. According to the COVID-19 status report (SITREP), the East Cameroon region documented its inaugural case of COVID-19 on April 08, 2020, thereby anchoring the study within the broader timeline of the pandemic’s emergence in the region.
Data Collection
Data collection took place between April 2019 and April 2021 that is, approximately for 25 months. We conducted a retrospective cohort study in selected health facilities in the East region of Cameroon [Figure 1]. These were as follows: Bertoua Regional Hospital, CSC Belabo, HD Abong Mbang, HD Messamena, HD Mbang, HD Lomié, PLT Batouri (Damien Foundation), CMA Kentzou, HD Yokadouma, HP Garoua Boulai, and HD Betare Oya (11 health facilities). The first step was to identify all HIV-TB coinfected patients from April 2019 to September 2019 and from May 2020 to October 2020 through the various registers in the TB Treatment Centers, UPECs, and CTAs of the health facilities. The second step was to manually examine the TB and antiretroviral therapy (ART) registers and the medical records of all HIV-TB coinfected patients. We selected a first cohort (CA) of patients declared coinfected from April 2019 to September 2019 before the occurrence of the first case of COVID-19 in the region (08 April 2019) and who continued their treatment 06 months later. Then, we selected a second cohort (CB) of patients declared coinfected from May 2020 to October 2020 after the occurrence of the first case of COVID-19 in the region. All coinfected patients under 18 years of age and incomplete records will be excluded from the study. The sociodemographic data and contact details of the patients included in the study were obtained from registers, patient records, and electronic medical records (EMRs) which is a software program used in certain health facilities in the Eastern region to monitor patients. The information was shared with 13 trained data collectors employed in the health facilities. Their task was to collect the information using Kobo Collect, an Android application that replaces the paper forms used to collect survey data. Data were collected at the patient’s appointment at the health facility or at the patient’s home.
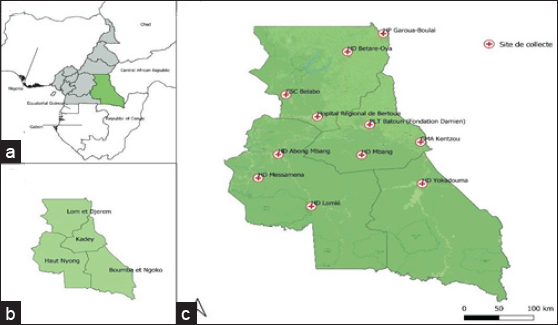
- Geographical representation of the study area. (a) Highlights the Eastern region, (b) highlights the departments of the Eastern region, and (c) highlights the data collection points in each department of the Eastern region.
Data Analysis
Data entered in the Kobo Collect application were downloaded and exported to a Microsoft Excel spreadsheet and imported into the Statistical Package for the Social Sciences (SPSS) version 23.0. Sociodemographic characteristics were analyzed by cohort, presented as proportions, and compared using Fisher’s exact test. Differences were considered significant when P < 0.05.
Ethical Considerations
The study was approved by the National Ethical Committee for Research on Human Health. Every precaution was taken to ensure that the rights of patients in the study were respected. We obtained verbal informed consent from patients ,and the study did not include personal details that could identify patients.
RESULTS
Table 2 shows that age, marital status, level of education, occupation, monthly income, religion, department, place of residence, and distance from home to the health facility are distributed in the same way between the cohort of patients before COVID and patients during COVID. However, sex (P = 0.010) and department (P = 0.021) are not distributed in the same way between the two types of cohort.
| Characteristics | n (%) | Cohort | P-value | |
|---|---|---|---|---|
| Before COVID (%) | During COVID (%) | |||
| Age (years) (mean ± SD) | 39.3 ± 11.4 | 40.0 ± 12.4 | 39.7 ± 10.3 | 0.563 |
| Gender | ||||
| Female | 111 (51.9) | 66 (60.6) | 45 (42.9) | 0.010 |
| Male | 103 (48.1) | 43 (39.4) | 60 (57.1) | |
| Marital status | ||||
| Single | 81 (38.2) | 48 (44.0) | 33 (38.2) | 0.089 |
| Divorced | 8 (3.8) | 6 (5.5) | 2 (1.9) | |
| Married | 106 (50.0) | 46 (42.2) | 60 (58.3) | |
| Widow(er) | 17 (8.0) | 9 (8.3) | 8 (7.8) | |
| Level of study | ||||
| None | 15 (7.1) | 10 (9.2) | 5 (4.9) | 0.121 |
| Primary | 95 (44.8) | 55 (50.5) | 40 (38.8) | |
| Secondary | 97 (45.8) | 42 (38.5) | 55 (53.4) | |
| Superior | 5 (2.4) | 2 (1.8) | 3 (2.9) | |
| Occupation | ||||
| Farmer/craftsman | 73 (34.3) | 40 (37.0) | 33 (31.4) | 0.486 |
| Trader | 69 (32.4) | 30 (27.8) | 39 (37.1) | |
| Unemployed | 45 (21.1) | 23 (21.3) | 22 (21.0) | |
| Worker | 26 (12.2) | 15 (13.9) | 11 (10.5) | |
| Monthly income | ||||
| <50 000 XAF | 97 (46.2) | 55 (50.5) | 42 (41.6) | 0.336 |
| 50 000–100 000 XAF | 95 (45.2) | 44 (40.4) | 51 (50.5) | |
| ≥100 000 XAF | 18 (8.6) | 10 (9.2) | 8 (7.9) | |
| Religion | ||||
| Christian | 159 (76.4) | 86 (78.9) | 73 (73.7) | 0.200 |
| No religion | 24 (11.5) | 14 (12.8) | 10 (10.1) | |
| Muslim | 25 (12.0) | 9 (8.3) | 16 (16.2) | |
| Residence | ||||
| Rural | 115 (53.7) | 61 (56.0) | 54 (51.4) | 0.506 |
| Urban | 99 (46.3) | 48 (44.0) | 51 (48.6) | |
| Distance from home/HF | ||||
| <10 km | 118 (55.1) | 60 (55.0) | 58 (55.2) | 0.977 |
| More than 10 km | 96 (44.9) | 49 (45.0) | 47 (44.8) | |
SD: Standard deviation, HF: Health Facility, XAF: Central African CFA Franc, n: number of patients, p-value <0.05 at 95% confidence interval was set as the cut-off point for any statistically significant association.
Table 3 shows the clinical characteristics of patients by cohort type. The results show that the patient status (P = 0.033) of the participants is not distributed in the same way in the two types of cohort (cohort before COVID-19 and cohort during COVID-19), whereas the other characteristics such as patient outcome, type of TB, TB treatment protocol, knowledge of duration of treatment, and adverse effects are distributed in the same way between the two types of cohort.
| Characteristics | n (%) | Cohort | P-value | |
|---|---|---|---|---|
| Before COVID-19 (%) | During COVID-19 (%) | |||
| Patient status | ||||
| New | 206 (96.3) | 108 (99.1) | 98 (93.3) | 0.033 |
| Relapse | 8 (3.7) | 1 (0.9) | 7 (6.7) | |
| Outcome of the patient | ||||
| Interruption of treatment | 9 (4.2) | 7 (6.4) | 2 (1.9) | 0.171 |
| On treatment | 205 (95.8) | 102 (93.6) | 103 (98.1) | |
| Type of tuberculosis | ||||
| Extrapulmonary | 31 (15.1) | 17 (16.7) | 14 (13.6) | 0.539 |
| Pulmonary | 174 (84.9) | 85 (83.3) | 89 (86.4) | |
| TB treatment protocol | ||||
| RH | 4 (2.3) | 2 (2.3) | 2 (2.2) | 1.0 |
| RHEZ | 171 (97.7) | 84 (97.7) | 87 (97.8) | |
| Knowledge of treatment duration | ||||
| Yes | 194 (94.6) | 97 (95.1) | 97 (94.2) | 0.769 |
| No | 11 (5.4) | 5 (4.9) | 6 (5.8) | |
| Undesirable effect | ||||
| Yes | 134 (65.4) | 67 (65.7) | 67 (65.0) | 0.924 |
| No | 71 (34.6) | 35 (34.3) | 36 (35.0) | |
n: number of patients, TB: Tuberculosis, p-value <0.05 at 95% confidence interval was set as the cut-off point for any statistically significant association. RH: Rifampicin and isoniazid, RHEZ: Pyrazinamid, rifampicin, isoniazid, and ethambutol.
Table 4 shows the family characteristics and habits of the patients by type of cohort. The results show that participants’ compliance with anti-COVID-19 barrier measures (P = 0.006) is not distributed in the same way in the two types of cohorts (cohort before COVID-19 and cohort during COVID-19). On the other hand, other characteristics, such as the attitude of the family/close friends toward the patient, assistance in taking medication, and drug use, were distributed in the same way between the two types of cohorts.
| Characteristics | n (%) | Cohort | P-value | |
|---|---|---|---|---|
| Avant COVID (%) | Pendant COVID (%) | |||
| Attitude of family and friends | ||||
| Discriminatory | 38 (18.5) | 18 (17.6) | 20 (19.4) | 0.744 |
| Not discriminatory | 167 (81.5) | 84 (82.4) | 83 (80.6) | |
| Help with taking medication | ||||
| Yes | 142 (69.3) | 71 (69.6) | 71 (68.9) | 0.916 |
| No | 63 (30.7) | 31 (30.4) | 32 (31.1) | |
| Drug use | ||||
| Yes | 18 (8.8) | 9 (8.8) | 9 (8.7) | 0.983 |
| No | 187 (91.2) | 93 (91.2) | 94 (91.3) | |
| Compliance with anti-COVID-19 barrier measures | ||||
| Yes | 38 (19.4) | 26 (27.4) | 12 (11.9) | 0.006 |
| No | 158 (80.6) | 69 (72.6) | 89 (88.1) | |
n: number of patients.
DISCUSSION
The aim of our study was to determine the prevalence and describe the epidemiological and clinical characteristics of HIV-TB coinfected patients in the COVID-19 context in health facilities in the East region of Cameroon. The prevalence of HIV-TB coinfection in our population was 1.28% (158/12,303) before the COVID-19 period and 0.74% (104/13,964) during the COVID-19 period. These results are lower than those of studies conducted in Nigeria, where the rate was 7.8%,[8] 27.7% in Ethiopia,[9] and 8.5% in Tanzania.[10] Variations in the rate of HIV-TB coinfection can be explained by the low rate of case reporting in some health facilities (under-reporting of cases), the lack of national reporting tools, the level of coverage of highly active ART, the lack of staff training in the detection of suspected TB cases among HIV patients, the diagnostic procedures used, differences in the diagnosis of TB, the epidemiology of TB in the different health facilities, and the research methodology applied to each study.
The lack of staff training in the detection of suspected TB cases among HIV patients could lead to underdiagnosis and subsequently lower reported coinfection rates. Diagnostic procedures, including the methods used to detect TB cases, may vary between regions and health facilities, influencing reported prevalence rates. Differences in the diagnosis of TB, ranging from screening protocols to laboratory techniques, can also contribute to variations in reported prevalence.
The epidemiology of TB itself varies across different health facilities and regions. Factors such as population density, socioeconomic conditions, and prevalence of other comorbidities can impact the incidence of TB, thus influencing the prevalence of HIV-TB coinfection. Finally, the methodological approaches applied in each study, including study design, sampling techniques, and data collection methods, can introduce variability in reported prevalence rates.
Our studys’ findings, while lower than those reported in some other regions, highlights the complex interplay of factors influencing the prevalence of HIV-TB coinfection. These factors underscore the importance of standardized reporting tools, comprehensive staff training, and consistent diagnostic procedures to ensure accurate and comparable prevalence data. Furthermore, our results emphasize the need for tailored interventions to address the unique challenges posed by the co-occurrence of HIV and TB, particularly in the context of the ongoing COVID-19 pandemic. Future research endeavors should continue to explore these complexities to inform targeted public health strategies for the management and prevention of HIV-TB coinfection.
The mean age was 39.3 ± 11.4 years, with a sex ratio of 1.33 in the cohort during COVID-19. Several authors have reached the same conclusions regarding male predominance.[11–14] In this case, young men are the most affected by the double burden of HIV and TB. They represent the most sexually active and productive segment of the population. The fact that there are more coinfected men than women could be explained by the fact that women in the region are tested for HIV earlier than men due to the necessity of HIV testing during pregnancy. This earlier testing provides women with the opportunity to be tested for TB in cases of HIV seropositivity, contributing to a potentially lower rate of coinfection in women. This observation highlights the interconnectedness of healthcare services, emphasizing the impact of HIV testing practices on the detection of TB cases and subsequent coinfection rates. Regarding marital status, our study identified a significant association between TB and married individuals, followed by single patients, while divorced or widowed patients were less likely to develop TB. This finding aligns with a study conducted by Mitku et al. in Ethiopia in 2016.[9] The association between TB and marital status may be attributed to lifestyle differences among various groups. Single patients, typically younger, may engage in different social behaviors that could elevate their risk of TB. Conversely, divorced or widowed individuals, potentially older and settled in different lifestyles, may exhibit a lower likelihood of TB development.
This study showed that around 93% of patients had at least primary school education. We found that there was no statistically significant association at the 5% significance level between educational level and adherence to treatment (P = 0.121). This result is contrary to the findings of Issoufi in 2008.[15] He observed that patients with a high level of education are associated with good adherence to programs to combat these diseases. Their various studies confirm this hypothesis. About 46.2% of patients have an income of <50,000 francs. Free treatment is fundamental to adherence, given the vulnerabilities associated with the social integration of people affected by the disease. Health services, therefore, need to pay particular attention to understanding patients’ needs.[16] In this study, the pulmonary location of TB was 84.9%, which is far from the result (56.5%) obtained by Soumaré et al. in Bamako.[13] This difference could be explained by the difficulty of diagnosing extrapulmonary TB, as the technical facilities are limited to microscopy, which makes it difficult to diagnose extrapulmonary forms. About 65.4% of patients surveyed stated that they had experienced adverse effects related to their treatment. This result is slightly different from the 42% obtained by Berkchi et al.[17] These adverse effects could be explained by the possible interaction between antiretroviral and anti- TB treatments.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
The results of this study are important because they highlight the high prevalence of HIV-TB coinfection in a specific population with a detailed presentation of certain sociodemographic characteristics. However, it is important to note that this study does not specifically address the clinical outcomes of this population. It provides a detailed presentation of the sociodemographic characteristics of an HIV-TB coinfected population in a specific context. Further research in this area is important to better understand the challenges associated with the diagnosis and treatment of HIV-TB coinfection, particularly in the context of the COVID-19 pandemic.
Key Messages
-
Hospital staff should improve the quality of documentation to enable assessment of whether the patient is attending regular medical consultations and recommended follow-up visits.
-
Health facilities should have a good policy for archiving patient information to ensure continuity of care, research, patient safety, and cost reduction by setting up an electronic patient file that eliminates the costs associated with paper records.
-
The pulmonary location of tuberculosis is the most common form among patients in the East region of Cameroon due to limited diagnostic facilities for extrapulmonary forms.
-
Many coinfected patients experience adverse effects related to their treatment, possibly due to interactions between antiretroviral and anti-tuberculosis medications.
Acknowledgments
The authors are grateful to all who took part in this study.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
There was no funding for this study.
Ethics Approval
Ethical approval for the study was sought and obtained from the National Ethical Committee for Research on Human Health on 4th September 2023, number 2023/08/1558/CE/CNERSH/SP.
Declaration of Patient Consent
Verbal informed consent was obtained from the patient.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
None.
REFERENCES
- HIV/AIDS report 2017: Joint United Nations Programme on HIV/AIDS (UNAIDS). Geneva: World Health Organization; 2016.
- Harrison’s principles of internal medicine (19th ed). New York: McGraw-Hill Education; 2015.
- The end TB strategy. Geneva: World Health Organization; 2014. [Accessed 2023 Nov 01]. Available from: https://www.who.int/teams/control-of-neglected-tropical-diseases/lymphatic-filariasis/morbidity-management-and-disability-prevention/global-tuberculosis-programme
- Global tuberculosis report. Geneva: World Health Organization; 2013. [Accessed 2023 Nov 01]. Available from: http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf
- [Accessed 2023 Sep 08]. Available from: https://www.who.int/fr/news-room/fact-sheets/detail/tuberculosis
- Rapport mondial sur la tuberculose 2021. Genève: Organisation Mondiale De La Santé; 2021. [Accessed 2023 Nov 01]. Available from: https://www.who.int/fr/publications-detail/9789240037021
- HIV testing, HIV status and outcomes of treatment for tuberculosis in a major diagnosis and treatment centre in Yaoundé, Cameroon: A retrospective cohort study. BMC Infect Dis. 2012;12:190.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence, and predictors of tuberculosis coinfection among HIV-seropositive patients attending the Aminu Kano Teaching Hospital, Northern Nigeria. J Epidemiol. 2009;19(2):81-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and associated factors of TB/HIV co-infection among HIV infected patients in Amhara Region, Ethiopia. Afr Health Sci. 2016;16(2):588-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulmonary tuberculosis among people living with HIV/AIDS attending care and treatment in rural Northern Tanzania. BMC Public Health. 2008;8:341.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of pulmonary bacilliferous tuberculosis according to the HIV status of patients followed in the infectious diseases Department of Conakry (Guinea) Bull Société Pathol Exot. 2014;107(5):346-9.
- [CrossRef] [PubMed] [Google Scholar]
- HIV/tuberculosis co-infection: epidemiological, clinical and therapeutic aspects of HIV/Tuberculosis co-infection in three communes of Bamako. Saarbrücken: Presses Académiques Francophones; 2013.
- TB/HIV co-infection: Tuberculosis in the era of HIV in Africa: The experience of the CHU du point-G. Rev Mal Respir. 2012;29:A197.
- [Google Scholar]
- Epidemioclinical and evolutionary aspects of tuberculosis and HIV co-infection in Cotonou. Médecine Mal Infect. 2012;42(11):561-6.
- [CrossRef] [PubMed] [Google Scholar]
- Study of Adherence to ARV Treatment of patients followed at Gao Hospital (Doctoral Thesis). Mali: University of Bamako; 2008.
- Representations on adherence to the treatment of multidrug-resistant tuberculosis. Rev Esc Enferm USP. 2018;52:e03412.
- [CrossRef] [PubMed] [Google Scholar]






