Translate this page into:
Sociodemographic and Health Determinants of Inequalities in Life Expectancy in Least Developed Countries
✉Corresponding author email: nazrulupm@gmail.com
Abstract
Background:
Life expectancy (LE) at birth is a widely used indicator of the overall development of a country. Therefore, we attempted to build up the relationships between sociodemographic and health factors with LE in the least developed countries (LDCs).
Methods:
Data and necessary information of 48 LDCs were obtained from the United Nations agencies. LE was the response variable and determinant factors were sociodemographic and health related variables. Stepwise multiple regression analysis was used to extract the main factors.
Results:
All predictors were found significantly correlated with LE. Finally, crude death rate, infant mortality rate, physicians density, and gross national income per capita were identified as the significant predicators of LE.
Conclusions:
The findings suggest that international efforts should be aimed at increasing LE by decreasing mortality rates, and increasing physicians density and national income in the LDCs.
Keywords
Life Expectancy
Least Developed Countries
Sociodemographic Determinants of Health Factors
Stepwise Multiple Regression
Global Disparities
Introduction
Life expectancy (LE) at birth refers to the number of years a person is expected to live based on the statistical average. It is a well-known demographic measure of population longevity and an important indicator for assessing socio-economic development of a region.[1] The level and variability of LE has important implications for individual and aggregate human behaviors. It affects fertility behavior, economic growth, human capital investment, intergenerational transfers, and incentives for pension benefit claims and vary according to gender and areas of residence.[2-3] LE reflects the health of a country's people and to what extent they receive quality care when they are ill.[4-5] It has increased significantly over the past half-century, but also demonstrated persistently high variability between countries. LE varies across the regions due to different patterns of poverty status and living arrangements.[6] In many of the countries of the developing world, particularly in Sub-Saharan Africa, LE has been decreased, although income and health expenditure are increasing.[7] Therefore, significant inequalities in LE still exist in the least developed countries (LDCs).
Recent studies have reported that LE is influenced by a number of sociodemographic and health factors and also identified the relationships between LE and the determinant factors.[8-14] A positive correlation between LE and gross domestic product (GDP), and negative correlations between LE and literacy rate, and proportion of population in rural China has been reported.[15] It has been demonstrated that longer LE is strongly associated with higher level of education and income.[16-17] A study in India found positive association between LE and per capita income, health expenditure, housing facility, availability of electricity, and telephone accessibility, whereas negative associations were found with some demographic variables like higher birth rate, death rate, and population growth rate.[18] However, another study on LE of developing countries reported that socioeconomic factors like per capita income, education, health expenditure, access to safe water, and urbanization cannot always be considered as the determinants of LE.[7] It has been established that the LE could be increased with the increase of healthcare services such as increased number of physicians, hospital deliveries, prenatal healthcare, and decrease Human Immunodeficiency Virus (HIV) prevalence, and mortalities.[8-9,19-21] The researches on quantifying the contributions of sociodemographic and health related parameters on LE have already been conducted for a country or many countries including low- and lower-middle-countries. However, no sound study was concentrated to identify the effects of sociodemographic and health factors on LE for the LDCs taken together. In this study, we attempt to fill up this gap in the literature. Therefore, the main objectives of this study are to build up the relationships between LE with sociodemographic, and health factors and to identify the most prominent determinant factors of LE.
Methods
The sociodemographic and health factors that had the significant effects on LE in the previous studies were considered for this study. Data and necessary information on 48 LDCs were obtained from the specialized agencies of the United Nations (UN) system, including the World Health Organization,[22] United Nations Development Programs,[23] and World Population Data Sheet, Population Reference Bureau.[24] The effective use of data for public policy is of critical importance to the UN in its efforts to strengthen evidence-based programming and policy development. The UN agencies rely on an extensive peer review process, which is conducted through leading regional and national statistics offices and international organizations, thus ensuring the level of data consistency and accuracy. Country list was taken from the United Nations Conference on Trade and Development.[25] The LDCs are the countries that, according to the UN, exhibit the lowest indicators of socioeconomic development, with the lowest Human Development Index ratings of all countries in the world. The concept of LDCs originated in the late 1960s and the first group of LDCs was listed by the UN in its resolution 2768 (XXVI) of 18 November 1971. The countries are classified as LDCs if they met three criteria: (i) poverty (adjustable criterion: three-year average gross national income (GNI) per capita of less than US $992, which must exceed $1,190 to leave the list as of 2012); (ii) human resource weakness (based on indicators of nutrition, health, education and adult literacy); and (iii) economic vulnerability (based on instability of agricultural production, instability of exports of goods and services, economic importance of non-traditional activities, merchandise export concentration, handicap of economic smallness, and the percentage of population displaced by natural disasters).[25] A list of the LDCs included in the study is shown in Table 1.
| Regions | n | Country |
|---|---|---|
| Africa | 33 | Angola, Benin, Burkina Faso, Burundi, Central African Republic, Chad, Comoros, Democratic Republic of the Congo, Djibouti, Equatorial Guinea, Eritrea, Ethiopia, Gambia, Guinea, Guinea-Bissau, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Mozambique, Niger, Rwanda, Sao Tome and Principe, Senegal, Sierra Leone, Somalia, Sudan, Togo, Uganda, United Republic of Tanzania, Zambia |
| Asia | 09 | Afghanistan, Bangladesh, Bhutan, Cambodia, Lao People's Democratic Republic, Myanmar, Nepal, Timor-Leste, Yemen |
| Americas | 01 | Haiti |
| Pacific | 05 | Kiribati, Samoa, Solomon Islands, Tuvalu, Vanuatu |
Note: n=Number of countries. aBased on the United Nations' geographical region
Variables and their description
The study investigated the effects of some sociodemographic and health factors on LE. The LE at birth is the main outcome variable of this study which is measured by the average number of years a newborn infant can expect to live under current mortality levels.[24] The determinants of LE are grouped into 2 main categories: sociodemographic indicators and health factors. The sociodemographic indicators were GNI per capita, educational index, adolescent fertility rate (AFR), total fertility rate (TFR), population density, infant mortality rate (IMR), and crude death rate (CDR); and the health factors were physicians density, HIV prevalence rate, and sanitation usage rate.
The GNI per capita is the GNI in purchasing power parity (PPP) divided by mid-year population, refers to GNI converted to international dollars using a PPP conversion factor.[24] International dollars (US $) indicate the amount of goods and services that one could buy in the United States of America with a given amount of money. The education index is calculated from the mean years of schooling index and the expected years of schooling index.[23] The AFR is the number of births to adolescent women (15-19 years) per 1,000 adolescent women; TFR is the average number of children that would be born to a woman by the time she ended her childbearing age (15-49 years) if she were to pass through all her childbearing years, and conforms to the age- specific fertility rates of a given year.[24] Physicians density is measured as the number of physicians per 10,000 populations of a particular area.[22] The HIV prevalence rate is estimated as the number of adults living with HIV/Acquired Immune Deficiency Syndrome (AIDS) per 100,000 populations of a particular area at a fixed period of time.[22] The IMR is the total number of deaths of infants (aged below one year) per 1,000 live births in a year or a period of time.[24] CDR is the total number of deaths per 1,000 populations in that population in a year.[24] Population density is the number of population per square kilometers of area,[24] and sanitation usage rate is the percentage of population using sanitation facilities.[22]
Statistical analysis
Univariate, bivariate, and multivariate analyses were performed for addressing the objectives. Univariate analysis was performed to analyze the selected variables in relation to maximum, minimum, mean, standard deviation (SD), median, and standard error of mean (SE mean). This analysis is useful as the study variables are often measured in diverse units. Pearson correlation analysis was used for the bivariate analysis. The correlation coefficients (r) were derived to examine direction, strength and significance of linear relationships between the study variables. Finally, forward multiple linear regression analysis was used to examine the average relationship between LE and the sociodemographic and health factors and to identify the most prominent factors of LE. In statistics, stepwise regression includes regression models in which the choice of predictive variables is carried out by an automatic procedure. Usually, this takes the form of a sequence of F-tests or t-tests, but other techniques are possible, such as adjusted R2, Akaike information criterion, Bayesian information criterion, Mallows's Cp, or false discovery rate. An impact analysis helps to standardize the effects of each independent variable on the dependent variable, and allows one to determine reasonably, which independent variable affects the dependent variable the most. The underlying multiple linear regression model corresponding to each variable is:
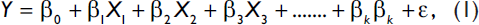
where, Y is the response variable (LE), X's (i =1,2, 3,...,k) are the predictors, β0 is the intercept term, βs (i =1, 2, 3,...,k) are the unknown regression coefficients, and ε is the error term with Ν(0,σ2) distribution. The variance inflation factor (VIF) was calculated to check multicolinearity problem among the predictors. The variance inflation for independent variables Xj is:
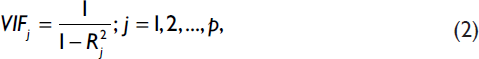
where, p is the number of predictors and Rj2 is the square of the multiple correlation coefficient of the j-th variable with the remaining (p-1) variables, where: (i) if 0<VIF<5, there is no evidence of a multicollinearity problem; (ii) if 5<VIF<10, there is a moderate multicollinearity problem; and (iii) if VIF>10, there is a serious multicollinearity problem of those variables. The Statistical Package for Social Sciences (SPSS) Version 20.0 (IBM SPSS Inc., Chicago, IL; USA) was used for statistical analysis.
Results
Univariate Analysis
The descriptive statistics of the variables under study are presented in Table 2, including the maximum and minimum values, as well as means, SDs, medians, and SE means. The results revealed that the LE at birth was found lowest in Sierra Leone (45 years) and highest in Samoa (73 years) among the LDCs. Most of the African countries had low LE, whereas LDCs from South East Asia and Pacific region had comparatively high LE like Bangladesh (70 years), Vanuatu (71 years), and Nepal (68 years). The average LE for these LDCs was 59.44 years. GNI was found the highest in Equatorial Guinea (US$ 18,900) and lowest in Congo (US$ 370). Among the Asian LDCs, GNI was lowest in Afghanistan (US$ 1,400) and highest in Timor-Leste (US$ 6,410) followed by Bhutan (US$ 6,310). However, the average GNI of 48 LDCs was US$ 2315.90. In case of education, the results showed that, majority of the Asian countries had lower education index compared to Pacific countries. However, Niger had the lowest education index (0.18) and Samoa had the highest (0.77), whereas the average education index for LDCs was 0.39. Most of the African countries had higher AFR among the selected LDCs like Niger (192 per 1,000) followed by Congo (168 per 1000) and Mali (167 per 1,000). In case of AFR, AFR of Myanmar was the lowest (12 per 1,000) and AFR of Niger was the highest (192 per 1,000). Similarly, TFR was also higher among African LDCs as Niger had highest TFR (7.60) followed by Chad (7.00) and Somalia (6.80). However, South Asian LDCs had relatively lower TFR like 2.30 in Bangladesh and 2.00 in Myanmar. In case of physicians density, the results showed that, African LDCs had lower physician density compared to Asian and Pacific LDCs. The physician density for all African LDCs were below 3.00 which mean that, for 10,000 people in those countries the number of available physicians was below 3. Even this number was very few for some countries like Malawi, Niger, Sierra Leone, and Tanzania. In Tanzania, there was only one physician per 100,000 people. HIV prevalence rate was found highest in African LDCs (14,619 per 100,000 populations in Lesotho, 7,204 per 100,000 populations in Zambia, and 5,904 per 100,000 populations in Malawi) and lowest in Asian LDCs (18 per 100,000 populations in Afghanistan and 5.10 per 100,000 populations in Bangladesh). However, IMR and CDR were found highest in African countries. The CDR was 5.00 in Samoa and Vanuatu, and 18.00 in Sierra Leone as compared with the average of 9.00 in LDCs. The similar trend was observed for IMR. In Sierra Leone, it was 128 per 1,000 live births, which was the highest among the LDCs. It was only 17 per 1,000 live births in Tuvalu, which was found the lowest. Population density was highest in Bangladesh (1,087 per square kilometers) and lowest in Mauritania (4 per square kilometers). Percentage of sanitation usage was very low in African LDCs (10.00% in Niger, and 11.00% in Togo).
| Variables | N | Minimum | Maximum | Mean±SD | Median | SE mean |
|---|---|---|---|---|---|---|
| Life expectancy | 48 | 45 | 73 | 59.44±6.56 | 60.00 | 0.95 |
| Gross national income | 44 | 370 | 18900 | 2315.90±2931.08 | 1505 | 441.88 |
| Educational index | 44 | 0.18 | 0.77 | 0.39±0.12 | 0.37 | 0.02 |
| Adolescent fertility rate | 46 | 12 | 192 | 83.70±43.61 | 69.50 | 6.43 |
| Total fertility rate | 48 | 2.00 | 7.60 | 4.83±1.28 | 4.90 | 0.18 |
| Physicians density | 37 | 0.10 | 10.90 | 1.65±2.00 | 1.00 | 0.33 |
| HIV prevalence rate | 41 | 5.10 | 14600 | 1716.10±2675.54 | 707 | 417.85 |
| Infant mortality rate | 48 | 17 | 128 | 63.19±24.02 | 61.00 | 3.47 |
| Crude death rate | 48 | 5.00 | 18.00 | 10.06±3.39 | 9.00 | 0.49 |
| Population density | 48 | 4.00 | 1087.00 | 116.40±181.88 | 50.50 | 26.25 |
| Sanitation usage rate | 45 | 10.00 | 92.00 | 36.49±21.00 | 33.00 | 3.13 |
Note: n=Number of countries, SE Mean=Standard error of mean, SD=Standard deviation
Bivariate analysis
The Pearson correlation coefficients (r) were used to examine the direction strength and significance of linear relationships between variables. The results of correlation coefficients (r) are presented in Table 3. The significant positive relationships were found between LE and education index (r = 0.39, P<0.01), physicians density (r = 0.49, P<0.01), population density (r = 0.29, P<0.05) sanitation usage rate (r = 0.49, P<0.01), and GNI (r = 0.07, P<0.05). On the other hand, significant converse relations were found between LE and AFR (r = -0.54, P<0.01), TFR (r = -0.58, P<0.01), HIV prevalence rate (r = -0.48, P<0.01), IMR (r = -0.08, P<0.01), and CDR (r = -0.95, P<0.01).
| Variables | (Y) | (X1) | (X2) | (X3) | (X4) | (X5) | (X6) | (X7) | (X8) | (X9) | (X10) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Life expectancy (Y) | 1.00 | ||||||||||
| Gross national income (X1) | 0.07* | 1.00 | |||||||||
| Educational index (X2) | 0.39** | 0.26 | 1.00 | ||||||||
| Adolescent fertility rate (X3) | −0.54** | −0.07 | −0.33* | 1.00 | |||||||
| Total fertility rate (X4) | −0.58** | −0.13 | −0.35* | 0.60** | 1.00 | ||||||
| Physicians density (X5) | 0.49** | 0.43* | 0.56** | −0.51** | −0.55** | 1.00 | |||||
| HIV prevalence rate (X6) | −0.48** | 0.03 | 0.29 | 0.13 | 0.05 | −0.42* | 1.00 | ||||
| Infant mortality rate (X7) | −0.083** | −0.16 | −0.38* | 0.34* | 0.52** | −0.52** | 0.11 | 1.00 | |||
| Crude death rate (X8) | −0.95** | −0.02 | −0.37* | 0.54** | 0.51** | −0.37* | 0.43** | 0.77** | 1.00 | ||
| Population density (X9) | 0.29* | −0.12 | 0.11 | −0.27 | −0.37** | 0.39* | −0.11 | −0.28 | −0.23 | 1.00 | |
| Sanitation usage rate (X10) | 0.49** | 0.49** | 0.44** | −0.56** | −0.39** | 0.62** | −0.08 | −0.36* | −0.42** | 0.31* | 1.00 |
Note: *significant at P<0.05 level, and **significant at P<0.01 level
Forward multiple regression analysis
The results of forward multiple regression analysis are presented in Table 4. The GNI, educational index, AFR, TFR, physicians density, HIV prevalence arte, IMR, CDR, population density, and sanitation usage rate were considered as predictors. In this analysis, four models (Model 1, Model 2, Model 3, and Model 4) were employed considering LE as the dependent variable. The VIF for all predictors were less than five, suggesting that there is no evidence of multicollinearity problem. In Model 1, only CDR was found as the significant predictor of LE (adjusted R2 = 0.91). In Model 2, CDR and IMR were found as the significant predictors of LE (adjusted R2 = 0.93). In Model 3, CDR, IMR, and physicians density were retained significant predictors where CDR and IMR were shown negative effects on LE; whereas, physicians density was shown positive impact on LE (adjusted R2 = 0.94). In Model 4, CDR, IMR, physicians density and GNI were found significant predictors (adjusted R2 = 0.95) where CDR and IMR were shown negative effects on LE and physicians density and GNI were shown positive impact on LE.
| Variables | Model 1 | VIF | Model 2 VIF | Model 3 | VIF | Model 4 | VIF |
|---|---|---|---|---|---|---|---|
| Crude death rate | −0.96** | 1.00 | −0.79** 2.41 | −0.78** | 2.44 | −0.730** | 2.67 |
| Infant mortality rate | −0.21* 2.41 | −0.19* | 2.46 | −0.21* | 2.48 | ||
| Physicians density | 0.11* | 1.13 | 0.12* | 1.15 | |||
| Gross national income | 0.11* | 1.12 | |||||
| Adjusted R2 | 0.91 | 0.93 | 0.94 | 0.95 |
Note: VIF: Variance inflation factor
Discussion
The LE is considered as one of the key early economic indicators. Poor and violent countries have low average life spans but high mortality and fertility rates. As economies improve, more money is spent on health care and services, and social safety nets are put in place. LE at birth is widely accepted as a useful indicator of the health status of a country's population and beyond that, international agencies use LE as a general indicator of national development. For LDCs, LE is not only important but also essential for development. In this study, we have identified all the sociodemographic and health factors under study as the significant predictors of LE. However, stepwise linear regression model identified that CDR, IMR, physicians density and GNI as the most prominent determinant factors of LE.
Economic development determines improvements in social conditions and increases LE. One measure of a country's standard of living is per capita GNI. This study consistently showed that GNI was strongly related to LE. There is considerable evidence linking income inequality to poor health outcomes. The LDCs obviously have less to spend on preventive medicine and healthcare, which might explain why average longevity is much shorter in such countries. This study established positive effects of GNI per capita on LE, which validates the previous study results.[8,27-28] Thus, economic upturns are associated with greater LE, and the opposite is true for economic downturns.
Education is also an important predictor of LE and we found that higher education levels among a population had a positive impact on LE. The correlation coefficient (r) for education index was statistically significant and similar. The higher education levels are associated with more timely receipt of healthcare and greater health awareness. People with more education are expected to be better responsive of the requirements to obtain enough prenatal care and can be encouraged to optimize the use of maternal healthcare, thereby avoiding childbirth-related complications such as low birth weight. The populations with more education typically earn higher real wages, which means that average household income is higher, allowing them to increase the quality and quantity of the healthcare services. Moreover, educated people usually tend to better understand information on proper nutrition, hygiene, healthcare services, and common illness prevention measures. Thus, it may be concluded that average LE will increase as education index increases.
Fertility decline is considered as the primary determinant of population ageing. The higher fertilities may have negative effects on LE since such families have limited resources per child especially in the LDCs. Moreover, a short period between births may terminate breast-feeding and endanger the nutritional status of infants.[29] In the present study, TFR and AFR were significantly inversely correlated with LE. The adolescents all over the world are exposed to excess reproductive-health hazards, as more than 14 million adolescents aged 15 to 19 years give births each year.[30] Moreover, AFR is strongly associated with adverse maternal and child health outcomes, including obstructed labor, low birth weight, fetal growth retardation, and high infant and maternal mortality.[31] In some cases higher fertilities refer to abuse of reproductive health rights of women.[32] The greater fertilities lead to higher prevalence of sexual activity; women and girls and expose them to unplanned pregnancies, unsafe abortions, and sexually transmitted diseases, including HIV.[33-35] Thus, less or delayed reproduction increases survivorship.
Availability of and access to healthcare services is an important factor in protecting against disease onset and accelerating recovery from illness and disability. We found that physicians density was significantly positively associated with LE. This is consistent with most previous researches in Western countries and highlights the important role that healthcare access plays in the survival of children and older people.[6,19] The greater healthcare availability in rural areas increases the better the survival and health conditions of the elderly.[21] In addition, maternal and fetal/neonatal survival depend on a continuum of basic services through pregnancy, delivery, and the neonatal period.[4] However, inadequate access to healthcare services for severe childhood illness could affect psychological development and accelerate declines in organ function during adulthood. These obstacles might reduce an individual's reserve capacity to resist disease, thus increasing mortality and health problems at later ages, leading to reduced LE. This might explain our findings regarding the association between physicians density and LE. Thus, it is established that the average LE will increase as the number of physicians per 10,000 people increases.
HIV is an incurable disease that ultimately attacks the immune system of infected individuals. Without treatment, net median survival time with HIV is 9 to 11 years, meaning that people with HIV have a much shorter life span. In this study, HIV prevalence rate is significantly inversely correlated with LE. The higher existence of infected adults could also mean the higher rates of potential HIV transmission.[34] So, the increased HIV prevalence rate corresponds to decreased LE. Many of the countries with high HIV prevalence rates experience a drop in LE.[36] The HIV epidemic continues to be associated with misconception and misinformed options that increase the risk of HIV transmission.[37] However, in the last decade, there has been a period of stagnation and inequalities in overall LE increased largely because of the decline in LE in sub-Saharan Africa, which was caused by the HIV epidemic.
The death rates (CDR and IMR) are significantly negatively correlated with LE. Mortality is the key indicator of health of a population. LE is a figure calculated from current death rates which tells us how long, on average, an individual of known age can expect to live if the population's death rates remain the same in the future. There may be the sub-groups of a population that suffer higher or lower death rates than the average. A population who is affected by the higher mortality can reveal differences in health status that can be addressed by suitable targeting of health services. Causes of deaths in the LDCs are extremely important. The infant and child mortalities are seen higher in the LDCs compared to other countries.[38-39] Consequently, the death rates are established as the driving factors for LE.
Human excreta have been implicated in the transmission of many infectious diseases including cholera, typhoid, infectious hepatitis, polio, cryptosporidiosis, and ascariasis. It has been estimated that about 1.80 million people die annually from diarrheal diseases where 90% are children under five, mostly in developing countries.[40] Poor sanitation gives many infections the ideal opportunity to spread: plenty of waste and excreta for the flies to breed on, and unsafe water to drink, wash with or swim in. Among human parasitic diseases, schistosomiasis ranks second behind malaria in terms of socioeconomic and public health importance in tropical and subtropical areas. Infection occurs with greatest frequency in tropical and subtropical regions, and in any areas with inadequate sanitation. Ascariasis is one of the most common human parasitic infections caused excreta. Infected individuals transmit trematode larvae in their feces. In many areas of Asia where trematode infections are endemic, untreated or partially treated excreta and night soil are directly added to ponds, rivers, or lakes.
Conclusions and Global Health Implications
Mortality is declining with time, which is a consequence of better conditions of life. A basic indicator of wellbeing is LE. Although increasing LE has been one of the significant global health achievements of the last century, however, the level of LE remains low in many LDCs. Sociodemographic and health factors predict LE. How sociodemographic and health factors affect LE in LDCs are analyzed in this study. We report that sociodemographic and health factors have significantly effects on LE. The results suggested that international efforts should pay attention to increasing LE in LDCs by increasing income and health facilities, improving situation and by decreasing deaths, fertilities and HIV prevalence rate. In this study, 48 LDCs were included and measured the effects of ten different determinants from sociodemographic and health factors. Further research with datasets that are more expansible and a wide range of factors would enhance policymakers' understanding of which factors influence LE the most.
Conflict of Interest:
The authors declare that they have no conflict of interest.
Ethical Consideration:
This paper is based on analysis of publicly-available secondary data.
Acknowledgements/Funding:
The authors are very grateful to the Department of Population Science and Human Resource Development, University of Rajshahi; Bangladesh has supported to complete the study. Thanks also to the editors and referees for their valuable comments and criticisms, which greatly improved this article.
References
- Impact of Life Expectancy on Economics Growth and Health Care Expenditures: A Case of Bangladesh. Universal Journal of Public Health. 2013;1(4):180-186.
- [CrossRef] [Google Scholar]
- Delays in claiming social security benefits. Journal of Public Economics. 2002;84:357-385.
- [CrossRef] [Google Scholar]
- Statistical evaluation of the life expectancy determining factors influence, vol. III, Globalization an. Higher Education in Economics and Business Administration (GEBA), Ed. Universităţii AlexandruloanCuza, Iaşi 2010:409-418.
- [Google Scholar]
- The gap gets bigger: changes on mortality and life expectancy, by education, 1981-2000. Health Affairs (Millwood). 2008;27(2):350-360.
- [CrossRef] [PubMed] [Google Scholar]
- The changing relation between education and life expectancy in central and eastern Europe in the 1990s. Journal of Epidemiology and Community Health. 2006;60:10-881.:875-881.
- [CrossRef] [PubMed] [Google Scholar]
- Remaining life expectancy among older people in a rural area of Vietnam: trends and socioeconomic inequalities during a period of multiple transitions. BMC Public Health. 2009;9:471.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Life Expectancy in Developing Countries. Journal of Developing Areas. 2008;41(2):185-204.
- [CrossRef] [Google Scholar]
- Relative Importance of Demographic, Socioeconomic and Health Factors on Life Expectancy in Low- and Lower- Middle- Income Countries. Journal of Epidemiology. 2014;24(2):117-124.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Socio-Health Factors on Life Expectancy in the Low and Lower Middle Income Countries. Iranian Journal of Public Health. 2013;42(12):1354-1362.
- [Google Scholar]
- Statistical Analysis of the Determinants of Life Expectancy in Romania. The Journal of the Romanian Regional Science Association. 2011;5(2):25-38.
- [Google Scholar]
- Factors affecting the HIV/ AIDS epidemic: an ecological analysis of global data. African Health Sciences. 2013;13(2):301-310.
- [CrossRef] [Google Scholar]
- Examining the relationship between life expectancy, reproduction, and educational attainment. Human Nature. 2010;21:269-289.
- [CrossRef] [Google Scholar]
- Decomposition of socioeconomic differences in life expectancy at birth by age and cause of death among 4 million South Korean public servants and their dependents. International Journal of Epidemiology. 2010;39:1656-1666.
- [CrossRef] [PubMed] [Google Scholar]
- Facing Up to Uncertain Life Expectancy: The Longevity Fan Charts. Demography2010;47(1):67-78.
- [CrossRef] [PubMed]
- Quantitative study on socioeconomic determinants of life expectancy in Beijing, China. Journal of Evidence Based Medicine. 2009;2(2):92-98.
- [CrossRef] [PubMed] [Google Scholar]
- Disability life expectancy for the elderly, city of Sao Paulo, Brazil, 2000: gender and educational differences. Journal of Biosocial Sciences. 2007;39(3):455-463.
- [CrossRef] [PubMed] [Google Scholar]
- Political and Social Determinants of Life Expectancy in Less Developed Countries: A longitudinal StudyBMC Public Health. 2012;12:85.
- [CrossRef] [PubMed]
- Principal Component Analysis of socioeconomic factors and their association with life expectancy in India. The Journal of Economics. 2013;113:163-172.
- [Google Scholar]
- Thai Cohort Study Team. Gender, socio-economic status, and self-rated health in a transitional middle- income setting: evidence from Thailand. Asia Pacific Journal of Public Health. 2011;23:754-765.
- [CrossRef] [PubMed] [Google Scholar]
- Life expectancy of Thai physicians during 1998-2002. Journal of Medical Association of Thailand. 2004;87(Suppl 4):S19-22.
- [Google Scholar]
- The determinants of life expectancy: an analysis of the OECD health data. South Economic Journal. 2005;71:768-783.
- [CrossRef] [Google Scholar]
- World Health Statistics 2013. World Health Organization (WHO) Geneva, Switzerland 2013
- [Google Scholar]
- The Least Developed Countries Report 2012: Harnessing Remittances and Diaspora Knowledge to Build Productive Capacities. In: United Nations Conference on Trade and Development (UNCTAD). 2013.
- [Google Scholar]
- The effect of health on economic growth: a production function approach. World Development. 2004;32(1):1-13.
- [CrossRef] [Google Scholar]
- Income inequality and health: importance of a cross country perspective. Social Science and Medicine. 2010;70:875-885.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology, evidence based medicine, and public health. Asia Pacific Journal of Public Health. 2009;21:244-251.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Breastfeeding Duration in Bangladesh. Asian Profile. 2013;41(3):263-270.
- [Google Scholar]
- Determinants of adolescent fertility in Ethiopia. Ethiopian Journal of Health Development. 2010;24(1):30-37.
- [CrossRef] [Google Scholar]
- Adolescent Fertility in the Developing World: Levels and Trends in the 1990's and Early 2000's. Paper presented at the annual meeting of the population association of America, Los Angeles, California, from March 30, 2006 to April I 2006
- [Google Scholar]
- Reproductive Health Rights of Women in the Rural Areas of Meherpur District in Bangladesh. Journal of Reproductive Infertility. 2011;12(1):23-32.
- [Google Scholar]
- Level of Awareness about HIV/AIDS among Ever Married Women in Bangladesh. Food and Public Health. 2012;2(3):73-78.
- [CrossRef] [Google Scholar]
- HIV/AIDS Acquisition and Transmission in Bangladesh: Turning to the Concentrated Epidemic. Japanese Journal of Infectious Diseases. 2009;62(2):111-119.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual Behavior and Sexually Transmitted Diseases in Street-based Female Sex Workers in Rajshahi City, Bangladesh. Brazilian Journal of Infectious Diseases. 2008;12(4):287-292.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with Misconceptions about HIV Transmission of Ever-Married Women in Bangladesh. Japanese Journal of Infectious Diseases. 2015;68:13-19.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Influencing Infant and Child Mortality: A Case Study of Rajshahi District, Bangladesh. Journal of Hum Ecology. 2009;26(1):31-39.
- [CrossRef] [Google Scholar]
- A Study on the Health Factors of Infant and Child Mortality in Rajshahi, Bangladesh. Asian Journal of Medical Sciences. 2009;1(3):82-87.
- [Google Scholar]
- World Health Statistics 2004. World Health Organization (WHO) 2004 Geneva, Switzerland
- [Google Scholar]





