Translate this page into:
Trends and Racial/Ethnic, Socioeconomic, and Geographic Disparities in Maternal Mortality from Indirect Obstetric Causes in the United States, 1999-2017
*Corresponding author e-mail: gsingh@hrsa.gov
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
This study examines trends and inequalities in US maternal mortality from indirect obstetric causes (ICD-10 codes: O98-O99) and specific chronic conditions by maternal race/ethnicity, socioeconomic status, nativity/immigrant status, marital status, place and region of residence, and cause of death.
Methods:
National vital statistics data from 1999 to 2017 were used to compute maternal mortality rates by sociodemographic factors. Rate ratios and log-linear regression were used to model mortality trends and differentials.
Results:
During 1999-2017, maternal mortality from indirect causes showed an upward trend; the annual rates increased by 11.2% for the overall population, 12.9% for non-Hispanic Whites, and 9.4% for non-Hispanic Blacks. The proportion of all maternal deaths due to indirect causes increased from 12.0% in 1999 to 26.9% in 2017. Maternal mortality from CVD increased sharply over time, from 0.40/100,000 live births in 1999 to 1.82 in 2017. During 2013-2017, compared to non-Hispanic Whites, non-Hispanic Blacks had 83% higher, Hispanics 51% lower, and Asian/Pacific Islanders 55% lower mortality from indirect causes. Non-Hispanic White women with <12 years of education had 4.4 times higher mortality than those with a college degree. Unmarried, US-born, and women living in rural areas and deprived areas had 90%, 80%, 60%, and 97% higher maternal mortality risks than married, immigrant, and women in urban areas and affluent areas, respectively. Maternal mortality from infectious diseases, including HIV, was 4.1 times greater and from respiratory diseases 2.9 greater among non-Hispanic Black women compared to non-Hispanic White women.
Conclusions and Global Health Implications:
While maternal mortality from direct obstetric causes has declined during the past two decades, maternal deaths due to indirect causes, particularly from pre-existing medical conditions, including CVD and metabolic disorders, have increased. Understanding complex interactions among social determinants, indirect causes, and proximate/direct causes is important to reducing maternal mortality and improving maternal health.
Keywords
Maternal mortality
Socioeconomic status
Deprivation
Race/ethnicity
Rural-urban
Disparities
Cause of death
Trend
1. Introduction
Although the leading causes of maternal deaths in the United States are hemorrhage, pregnancy-related hypertension, embolism, and obstetric infection, maternal deaths due to indirect obstetric causes, including chronic medical conditions such as cardiovascular disease (CVD), diabetes, respiratory disorders, and mental health conditions, have increased substantially in the past two decades.1,2 Globally, including the United States, 25-30% of all maternal deaths are attributed to these indirect causes.3-5 Recent trends and socioeconomic and demographic disparities in US maternal mortality from indirect causes have not been well studied, although the proportionate share of various indirect causes to overall mortality and racial/ethnic patterns have been examined using death certificate-based maternal mortality and Pregnancy Mortality Surveillance System data.6-9 To our knowledge, none of the US studies have analyzed inequalities in maternal mortality from indirect causes by a wide range of social determinants, including maternal education, marital status, nativity/immigrant status, place of residence, geographic region, and area deprivation. Analyzing disparities according to these social determinants is important in identifying sociodemographic groups and disadvantaged communities that may be at increased risk of maternal morbidity and mortality and which can benefit from targeted social and public heath interventions.
To address the aforementioned gaps in research, we analyzed racial/ethnic, socioeconomic, demographic, rural-urban, and regional variations in US maternal mortality from indirect obstetric causes and specific chronic conditions (ICD-10 codes O98-O99) occurring during or within 42 days after the end of pregnancy.1,2,10
2. Methods
We used 1999-2017 data from the National Vital Statistics System, the national mortality database.1,2,10 Maternal deaths in this study, are defined in accordance with the WHO as those related to or aggravated by pregnancy or pregnancy management and which occur during or within 42 days after the end of pregnancy.1,2,10 This official definition of maternal mortality differs from the definition of pregnancy-related mortality, which includes deaths during or within 1 year of pregnancy.8,9
Rates of maternal mortality from indirect causes were computed annually between 1999 and 2017 for all races, Whites and Blacks. Maternal deaths and rates for Asian and Pacific Islanders (APIs), American Indians and Alaska Natives (AIANs) and Hispanics, maternal education, marital status, nativity/immigrant status, and maternal age were derived using the pooled 5-year mortality and natality data for the period 2013-2017 because of the small numbers of maternal deaths annually and to produce statistically robust estimates for these demographic groups. The numbers of births by these sociodemographic characteristics, obtained from the national natality files, served as the denominators for computing maternal mortality rates.11
Area-based socioeconomic patterns in maternal mortality were derived by linking the 2008-2012 census-based county-level deprivation index to the race- and county-specific mortality statistics from 2013 to 2017.12-15 We used previously developed factor-based area deprivation index (ADI), developed by Singh and colleagues, using data from the 2008-2012 American Community Survey.12-15 The ADI consisted of 21 census-based socioeconomic indicators, which may be viewed as broadly representing educational opportunities, labor force skills, economic, and housing conditions in a given county.12-15 Selected indicators of education, occupation, wealth, income distribution, unemployment rate, poverty rate, and housing quality were used to construct these indices by factor and principal components analyses.12-15 The factor loadings (correlations of indicators with the ADI) for the 2008-2012 county index varied from 0.91 for 150% of the poverty rate to 0.23 for home ownership rate.12,15 To compute maternal mortality rates by deprivation level, we used the weighted population quintile distribution of the deprivation index that classified all 3,141 US counties into 5 groups of approximately equal population size.12-15 The groups thus created ranged from being the most-deprived (first quintile) to the least-disadvantaged (fifth quintile) population groups.12-15 To simplify analysis and for statistical robustness, we combined 2nd, 3rd, and 4th quintiles as the middle deprivation category. Each of the 3,141 counties in the mortality database was assigned one of these 3 deprivation quintiles.
Log-linear regression models were used to estimate annual rates of change in maternal mortality from indirect causes.13-15 Specifically, the logarithm of mortality rates were modeled as a linear function of time (calendar year), which yielded annual exponential rates of change in mortality rates.13-15 Disparities in mortality by social factors and deprivation level were described by rate ratios (relative risks=RR) and rate differences (absolute inequalities), which were tested for statistical significance at the 0.05 level.
3. Results
3.1. Trends in Maternal Mortality from Indirect Causes
Maternal mortality from indirect causes showed an upward trend during 1999-2017, with the rate increasing by 11.2% (95% CI=9.0%-13.5%) annually for the overall population, 12.9% (95% CI=10.5%-15.3%) for non-Hispanic Whites, and 9.4% (95% CI=7.2%-11.6%) for non-Hispanic Blacks (Figure 1). During 1999-2017, non-Hispanic Black women had 2-3 times higher mortality from indirect causes than non-Hispanic White women. The proportion of all maternal deaths due to indirect causes rose from 12.0% in 1999 to 26.9% in 2017 (Figure 2). Of 12,135 maternal deaths that occurred during 1999-2017, 3184 deaths were from indirect causes, including 173 deaths from maternal infectious and parasitic diseases, 3011 deaths from all chronic conditions, 993 deaths from CVD, 178 deaths from mental disorders, 191 deaths from respiratory diseases, 48 deaths from digestive diseases, 26 deaths from endocrine/metabolic disorders, and 30 deaths from HIV (Table 1). Maternal mortality from CVD increased sharply over time, from 0.40 per 100,000 live births deaths in 1999 to 1.82 in 2017 (Figure 1). During 1999-2017, the average annual rate of increase in maternal mortality was 8.8% (95% CI=7.0%-10.6%) for CVD, 11.3% (95% CI=8.9%-13.7%) for all chronic conditions combined, and 10.0% (95% CI=7.2%-13.0%) for infectious and parasitic diseases (Figures 1 and 2). Trends from other causes are not shown because of small numbers of deaths.
| Cause of death (ICD-10 codes) | Maternal | Maternal |
|---|---|---|
| Deaths | Mortality Rate | |
| All indirect causes (O98-O99) | 3,184 | 4.14 |
| Maternal infectious and parasitic diseases (O98) | 173 | 0.22 |
| Tuberculosis (O98.0) | 9 | N/A |
| Syphilis, Gonorrhea, and other sexually transmitted infections (O98.1-O98.3) | 2 | N/A |
| Viral hepatitis (O98.4) | 5 | N/A |
| Other viral diseases (O98.5) | 12 | 0.02 |
| Protozoal diseases (O98.6) | 0 | N/A |
| HIV (O98.7) | 30 | 0.04 |
| Other maternal infectious and parasitic diseases (O98.8) | 115 | 0.15 |
| Unspecified maternal infectious and parasitic diseases (O98.9) | 0 | N/A |
| Chronic diseases (O99) | 3,011 | 3.91 |
| Anemia (O99.0) | 22 | 0.03 |
| Blood & immune disorders (O99.1) | 24 | 0.03 |
| Endocrine and metabolic disorders (O99.2) | 26 | 0.03 |
| Mental disorders and diseases of the nervous system (O99.3) | 178 | 0.23 |
| Cardiovascular diseases (O99.4) | 993 | 1.29 |
| Respiratory diseases (O99.5) | 191 | 0.25 |
| Digestive system diseases (O99.6) | 48 | 0.06 |
| Skin and subcutaneous disorders (O99.7) | 5 | N/A |
| Other specified diseases and conditions (O99.8) | 1,524 | 1.98 |
Source: Derived from the National Mortality and Natality Detail Files, 1999-2017 Maternal mortality rates based on fewer than 10 deaths are not shown because of high variability associated with those rates. N/A = not available
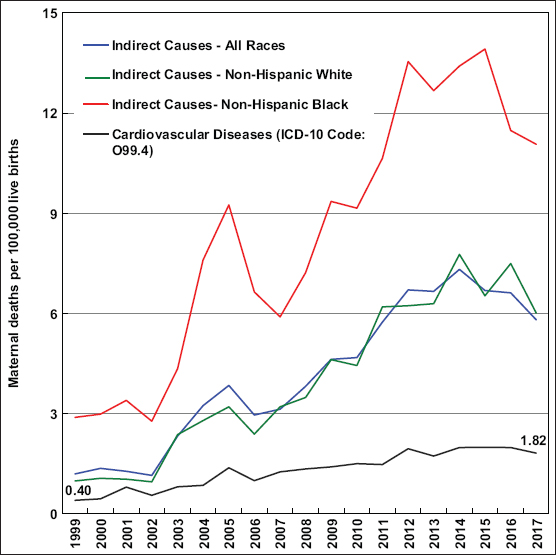
- Trends in maternal mortality from indirect obstetric causes (ICD-10 Codes: O98-O99), United States, 1999-2017
- Source: Data derived from the National Vital Statistics System.
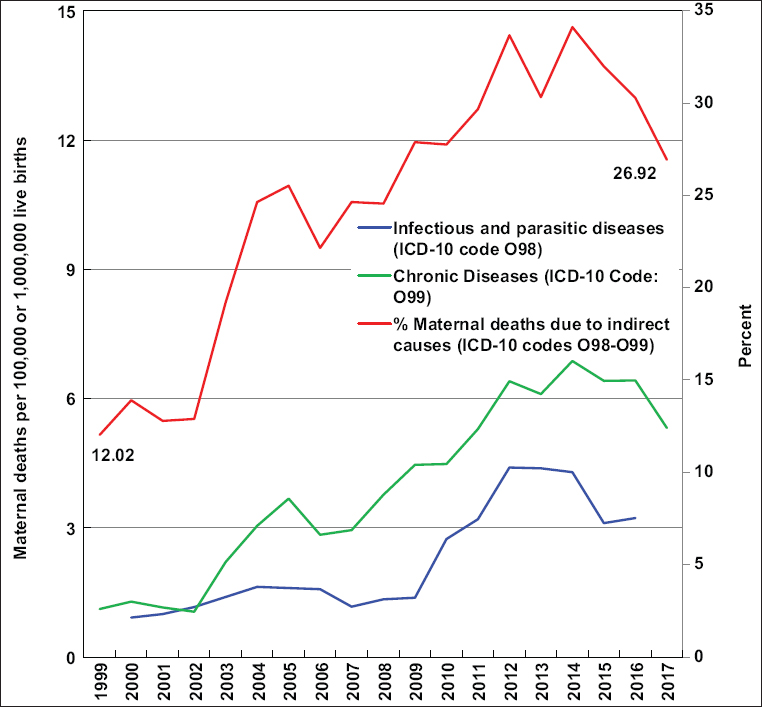
- Trends in maternal mortality from infections (ICD-10 code O98) and chronic diseases (ICD-10 code O99), and proportion of all maternal deaths due to indirect obstetric causes (ICD-10 codes: O98-O99), United States, 1999-2017
- Source: Data derived from the National Vital Statistics System
- Rates of maternal mortality from infections are three-year moving average rates and are per 1,000,000 (million) live births. Rates of maternal mortality from chronic diseases are annual rates and are per 100,000 live births.
3.2. Inequalities in Maternal Mortality from Indirect Causes by Sociodemographic Factors
During 2013-2017, mortality from indirect causes increased consistently with increasing maternal age, with relative risk of mortality being 17.9 times (76.76/4.28) higher for women aged ≥40 years than for those aged <20 (Table 2). Non-Hispanic Blacks had 83% higher (RR=1.83; 95% CI=1.60-2.06) and Hispanics 51% lower (RR=0.49; 95% CI=0.41-0.58) mortality from indirect causes than non-Hispanic Whites. Compared to APIs, non-Hispanic Whites, non-Hispanic Blacks, and AIANs had 2.2 times higher (RR=2.22; 95% CI=1.54-2.89), 4.1 times higher (RR=4.06; 95% CI=2.79-5.33), and 3.1 times higher (RR=3.09; 95% CI=1.48-4.70) mortality from indirect causes, respectively.
| Demographic variable | All races maternal deaths | All races number of live births | All races maternal mortality rate | NH White maternal deaths | NH white number of live Births | NH White maternal mortality rate | NH black maternal deaths | NH Black number of live births | NH Black maternal mortality rate | Hispanic maternal deaths | Hispanic number of live births | Hispanic maternal mortality rate |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternal age | ||||||||||||
| <20 | 50 | 1,168,621 | 4.28 | 22 | 456,900 | 4.82 | 13 | 260,307 | 4.99 | 11 | 408,367 | 2.69 |
| 20-24 | 146 | 4,198,579 | 3.48 | 76 | 1,978,431 | 3.84 | 41 | 864,004 | 4.75 | 25 | 1,160,512 | 2.15 |
| 25-29 | 206 | 5,691,179 | 3.62 | 107 | 3,158,790 | 3.39 | 66 | 826,627 | 7.98 | 21 | 1,262,475 | 1.66 |
| 30-34 | 229 | 5,415,637 | 4.23 | 118 | 3,198,425 | 3.69 | 65 | 599,400 | 10.84 | 29 | 1,028,383 | 2.82 |
| 35-39 | 211 | 2,622,901 | 8.04 | 119 | 1,441,324 | 8.26 | 55 | 303,462 | 18.12 | 30 | 554,553 | 5.41 |
| 40+ | 463 | 603,212 | 76.76 | 277 | 299,454 | 92.50 | 127 | 79,115 | 160.53 | 38 | 142,067 | 26.75 |
| All ages | 1,305 | 19,700,129 | 6.62 | 719 | 10,533,324 | 6.83 | 367 | 2,932,915 | 12.51 | 154 | 4,556,357 | 3.38 |
| Maternal education1 | ||||||||||||
| <12 years | 175 | 2,183,696 | 8.01 | 79 | 604,099 | 13.08 | 41 | 322,009 | 12.73 | 51 | 1,134,894 | 4.49 |
| 12 years | 420 | 4,310,035 | 9.74 | 230 | 1,993,110 | 11.54 | 126 | 857,512 | 14.69 | 43 | 1,233,191 | 3.49 |
| 13-15 years | 279 | 4,369,295 | 6.39 | 146 | 3,079,823 | 4.74 | 89 | 948,012 | 9.39 | 31 | 1,068,122 | 2.90 |
| 16+ years | 195 | 4,802,830 | 4.06 | 121 | 4,101,778 | 2.95 | 46 | 461,563 | 9.97 | 11 | 534,346 | 2.06 |
| RR (low/high education) | 1.97 (1.57-2.38) | 4.43 (3.18-5.69) | 1.28 (0.74-1.81) | 2.18 (0.76-3.60) | ||||||||
| Marital status2 | ||||||||||||
| Married | 493 | 11,496,272 | 4.29 | 305 | 7,368,124 | 4.14 | 85 | 858,295 | 9.90 | 72 | 2,045,025 | 3.52 |
| Unmarried | 628 | 7,716,306 | 8.14 | 294 | 3,027,397 | 9.71 | 230 | 2,043,382 | 11.26 | 75 | 2,286,040 | 3.28 |
| RR (unmarried/married) | 1.90 (1.67-2.12) | 2.35 (1.97-2.72) | 1.14 (0.85-1.42) | 0.93 (0.63-1.23) | ||||||||
| Nativity/immigrant status2 | ||||||||||||
| US-born | 970 | 15,240,735 | 6.36 | 575 | 9,930,504 | 5.79 | 300 | 2,499,661 | 12.00 | 66 | 2,328,713 | 2.83 |
| Foreign-born | 157 | 4,443,057 | 3.53 | 26 | 708,301 | 3.67 | 19 | 452,563 | 4.20 | 81 | 2,222,324 | 3.64 |
| RR (foreign-born/US-born) | 0.56 (0.46-0.65) | 0.63 (0.38-0.88) | 0.35 (0.19-0.51) | 1.29 (0.87-1.70) | ||||||||
| Place of residence | ||||||||||||
| Metro (urban) | 1,043 | 17026691 | 6.13 | 531 | 8434231 | 6.30 | 329 | 2758825 | 11.93 | 135 | 4744212 | 2.85 |
| Non-Metro (rural) | 262 | 2673438 | 9.80 | 188 | 1879286 | 10.00 | 38 | 287276 | 13.23 | 19 | 364094 | 5.22 |
| RR (non-metro/metro) | 1.60 (1.38-1.82) | 1.59 (1.32-1.85) | 1.11 (0.74-1.48) | 1.83 (0.95-2.71) | ||||||||
| Geographic region | ||||||||||||
| Northeast | 194 | 3,135,978 | 6.19 | 90 | 1,784,944 | 5.04 | 58 | 423,627 | 13.69 | 30 | 610809 | 4.91 |
| Midwest | 287 | 4,142,090 | 6.93 | 197 | 2,897,115 | 6.80 | 63 | 586,531 | 10.74 | 15 | 425090 | 3.53 |
| South | 691 | 7,635,103 | 9.05 | 348 | 3,807,352 | 9.14 | 239 | 1,680,107 | 14.23 | 83 | 1756884 | 4.72 |
| West | 133 | 4,786,958 | 2.78 | 84 | 2,043,913 | 4.11 | <10 | 242,650 | 2.88 | 26 | 1763574 | 1.47 |
| RR (South/West) | 3.26 (2.65-3.86) | 2.22 (1.69-2.75) | 4.93 (1.23-8.65) | 3.20 (1.80-4.63) | ||||||||
| Cause of death | ||||||||||||
| Infections (O98) | 78 | 19,700,129 | 0.40 | 29 | 10,533,324 | 0.28 | 34 | 2,932,915 | 1.16 | <10 | 4,556,357 | 0.20 |
| HIV | 24 | 19,700,129 | 0.12 | N/A | 19 | 2,932,915 | 0.65 | N/A | ||||
| Chronic diseases (O99) | 1,227 | 19,700,129 | 6.23 | 690 | 10,533,324 | 6.55 | 333 | 2,932,915 | 11.35 | 145 | 4,556,357 | 3.18 |
| Mental disorders (O99.3) | 86 | 19,700,129 | 0.44 | 60 | 10,533,324 | 0.57 | 17 | 2,932,915 | 0.58 | <10 | 4,556,357 | 0.18 |
| CVD (O99.4) | 374 | 19,700,129 | 1.90 | 189 | 10,533,324 | 1.79 | 120 | 2,932,915 | 4.09 | 41 | 4,556,357 | 0.90 |
| Respiratory diseases (O99.5) | 62 | 19,700,129 | 0.31 | 28 | 10,533,324 | 0.27 | 23 | 2,932,915 | 0.78 | 10 | 4,556,357 | 0.22 |
Source: Derived from the National Mortality and Natality Detail Files, 2013-2017. NH = Non-Hispanic; RR = relative risk or rate ratio. SE (Mortality Rate) ≈ Rate/SQRT(Deaths). The 5-year pooled mortality statistics for APIs: 44 deaths and a rate of 3.08 (95% CI=2.17-6.75) per 100,000 live births; for AIANs: 21 deaths and a rate of 9.52 (95% CI=5.45-13.59). Foreign-born or immigrants are defined as those born outside the 50 states and the District of Columbia in both natality and mortality files.
Higher educational attainment was associated with lower maternal mortality from indirect causes. Non-Hispanic white women with <12 years of education had 4.4 times higher mortality than their counterparts with a college degree. Unmarried, US-born, and women in rural areas had 90%, 80%, and 60% (RR=1.90, 1.80, 1.60) higher risks of maternal mortality from indirect causes than married, immigrant, and women in urban areas, respectively. Women in the southern region had 3.3 times higher mortality risk from indirect causes than those in the western region of the US.
Maternal mortality related to infectious diseases, including HIV, was 4 times greater among non-Hispanic Black women than non-Hispanic White women (Table 2; data not shown). Compared to non-Hispanic White women, maternal mortality from all chronic conditions combined and from CVD was approximately two times higher among black women but 50% lower among Hispanics. The risk of maternal death due to poor mental health was similar in both non-Hispanic White and Black women but significantly higher compared with that for Hispanic women. Maternal mortality due to respiratory conditions was 2.9 times greater among non-Hispanic Black women than non-Hispanic White women.
3.5. Inequalities in Maternal Mortality from Indirect Causes by Area Deprivation Index
During 2013-2017, women in the middle- and most-deprived area groups had 23% (RR=1.23; 95% CI=1.03-1.43) and 97% (RR=1.97; 95% CI=1.63-2.32) higher risks of maternal mortality from indirect causes than women in the most-affluent area group (Table 3). An approximately two-fold increased risk of maternal mortality from indirect causes was found among Non-Hispanic White and Black women living in the most-deprived areas (Table 3). When disparities across race/ethnicity and deprivation level were considered, maternal mortality rates from indirect causes varied greatly from 3.23 and 5.65 for Hispanics and non-Hispanic Whites in the most affluent area-group to 14.45 per 100,000 for non-Hispanic Blacks in the most deprived area-group (a 4.5-fold ethnic inequality). Patterns in maternal mortality by deprivation level were similar for all chronic conditions combined and for CVD, with women in the most deprived area-group experiencing about twice the mortality risk of those in the most affluent area-group (Table 3).
| Area deprivation Index | Maternal | Number of | Maternal | Maternal | 95% CI |
|---|---|---|---|---|---|
| Deaths | Live Births | Mortality | Mortality | ||
| Rate | RR | ||||
| All indirect causes (ICD codes: O98-O99) | |||||
| All races | |||||
| Ist quintile (low SES) | 389 | 3,982,978 | 9.77 | 1.97 | 1.63-2.32 |
| 2nd-4th quintile (middle SES) | 730 | 11,959,599 | 6.10 | 1.23 | 1.03-1.43 |
| 3rd quintile (high SES) | 186 | 3,757,363 | 4.95 | 1.00 | Reference |
| Non-Hispanic White | |||||
| Ist quintile (low SES) | 215 | 1,966,293 | 10.93 | 1.93 | 1.50-2.37 |
| 2nd-4th quintile (middle SES) | 385 | 6,572,306 | 5.86 | 1.04 | 0.82-1.25 |
| 3rd quintile (high SES) | 119 | 2,105,188 | 5.65 | 1.00 | Reference |
| Non-Hispanic Black | |||||
| Ist quintile (low SES) | 115 | 796,033 | 14.45 | 1.82 | 1.10-2.54 |
| 2nd-4th quintile (middle SES) | 221 | 1,771,290 | 12.48 | 1.57 | 0.98-2.16 |
| 3rd quintile (high SES) | 31 | 389,812 | 7.95 | 1.00 | Reference |
| Hispanic | |||||
| Ist quintile (low SES) | 40 | 1,024,822 | 3.90 | 1.21 | 0.60-1.82 |
| 2nd-4th quintile (middle SES) | 90 | 2,789,575 | 3.23 | 1.00 | 0.55-1.45 |
| 3rd quintile (high SES) | 24 | 741,950 | 3.23 | 1.00 | Reference |
| All chronic diseases (ICD code: O99) | |||||
| All races | |||||
| Ist quintile (low SES) | 362 | 3,982,978 | 9.09 | 1.91 | 1.57-2.25 |
| 2nd-4th quintile (middle SES) | 686 | 11,959,599 | 5.74 | 1.21 | 1.01-1.40 |
| 3rd quintile (high SES) | 179 | 3,757,363 | 4.76 | 1.00 | Reference |
| Non-Hispanic White | |||||
| Ist quintile (low SES) | 202 | 1,966,293 | 10.27 | 1.83 | 1.41-2.25 |
| 2nd-4th quintile (middle SES) | 370 | 6,572,306 | 5.63 | 1.00 | 0.80-1.21 |
| 3rd quintile (high SES) | 118 | 2,105,188 | 5.61 | 1.00 | Reference |
| Non-Hispanic Black | |||||
| Ist quintile (low SES) | 106 | 796,033 | 13.32 | 2.00 | 1.14-2.85 |
| 2nd-4th quintile (middle SES) | 201 | 1,771,290 | 11.35 | 1.70 | 1.01-2.40 |
| 3rd quintile (high SES) | 26 | 389,812 | 6.67 | 1.00 | Reference |
| Hispanic | |||||
| Ist quintile (low SES) | 38 | 1,024,822 | 3.71 | 1.15 | 0.56-1.74 |
| 2nd-4th quintile (middle SES) | 83 | 2,789,575 | 2.98 | 0.92 | 0.50-1.34 |
| 3rd quintile (high SES) | 24 | 741,950 | 3.23 | 1.00 | Reference |
| Cardiovascular diseases (ICD code: O99.4) | |||||
| All races | |||||
| Ist quintile (low SES) | 108 | 3,982,978 | 2.71 | 2.17 | 1.57-2.38 |
| 2nd-4th quintile (middle SES) | 219 | 11,959,599 | 1.83 | 1.46 | 1.57-2.38 |
| 3rd quintile (high SES) | 47 | 3,757,363 | 1.25 | 1.00 | Reference |
| Non-Hispanic White | |||||
| Ist quintile (low SES) | 51 | 1,966,293 | 2.59 | 1.76 | 0.98-2.55 |
| 2nd-4th quintile (middle SES) | 107 | 6,572,306 | 1.63 | 1.11 | 0.67-1.55 |
| 3rd quintile (high SES) | 31 | 2,105,188 | 1.47 | 1.00 | Reference |
| Non-Hispanic Black | |||||
| Ist quintile (low SES) | 38 | 796,033 | 4.77 | 2.06 | 0.56-3.57 |
| 2nd-4th quintile (middle SES) | 73 | 1,771,290 | 4.12 | 1.78 | 0.55-3.02 |
| 3rd quintile (high SES) | <10 | 389,812 | 2.31 | 1.00 | Reference |
Source: Derived from the National Mortality and Natality Detail Files and American Community Survey, 2013-2017. RR = relative risk or rate ratio. SE (Mortality Rate) ≈ Rate/SQRT(Deaths). Cardiovascular disease mortality rates for Hispanics are not shown because of small numbers of deaths. Maternal mortality rates based on fewer than 10 deaths are not shown because of high variability associated with those rates
4. Discussion
Using national vital statistics mortality data from 1999 to 2017, we found a rising trend in US maternal mortality from indirect causes, including CVD and all chronic conditions combined. The proportion of all maternal deaths due to indirect causes increased from 12.0% in 1999 to 26.9% in 2017, with maternal mortality from CVD increasing almost 5-fold during this time period. Our study shows marked disparities in maternal mortality from indirect causes by a wide array of social determinants, including maternal education, marital status, immigrant status, place of residence, geographic region, and area deprivation, which, although shown previously for overall maternal mortality and pregnancy-related mortality8,9,16, had not been documented for mortality from indirect causes to the best of our knowledge. Analysis of a broad range of disparities is important in showing the potential for reductions in US maternal mortality that can be achieved by implementing effective policies and interventions among high-risk groups and communities.
Efforts to reduce maternal mortality in the United States should be focused on indirect obstetric causes, in addition to addressing direct complications of pregnancy and childbirth.3,5,8,9 While maternal mortality from direct obstetric causes such as hemorrhage, pregnancy-related hypertension, and embolism has declined during the past two decades, maternal deaths due to indirect causes, particularly from pre-existing medical conditions, including CVD and metabolic disorders have risen.1-4,8,9 Given the increasing relative importance of indirect maternal causes of death, increased attention should be given to the healthcare needs of pregnant women with pre-existing conditions and high-risk pregnancies.5,17 Tackling the rising prevalence of obesity, diabetes, chronic hypertension, kidney diseases, and cardiovascular conditions among women of reproductive age should become a priority.3,5
Trends and social inequalities in mortality from indirect causes reported here are generally consistent with those observed for maternal mortality overall (direct + indirect causes), pregnancy-related mortality, various risk factors, chronic medical conditions, and maternal complications including pre-pregnancy obesity, maternal diabetes, chronic hypertension, poor mental health, and cardiovascular conditions among women of reproductive age.8,9,16,18,19 For example, consistent with patterns in maternal mortality from indirect causes in our study, a recent study of the 2012-2014 US birth cohorts found that the risk of pre-pregnancy obesity was significantly higher among non-Hispanic Blacks, AIANs, non-Hispanic Whites, unmarried, US-born, women aged ≥35, women with less education, and rural residents.20 Mothers with less than a high school or with a high school diploma had more than twice the risk of pre-pregnancy obesity than those with a college degree, and US-born women had 59% higher risk than immigrant women20 – estimates similar to those reported in our study on maternal mortality from indirect causes.
Another recent US study showed marked disparities in maternal hypertension (consisting of both chronic hypertension and pregnancy-related hypertension) by various social determinants.19 AIANs, non-Hispanic Blacks, and Pacific Islanders had higher risks of maternal hypertension and chronic hypertension, whereas Asians, Hispanics, and non-Hispanic Whites had lower risks of maternal hypertension, including chronic hypertension.19 Increasing maternal age, lower education, US-born status, rural residence, pre-pregnancy obesity, excess weight gain during pregnancy, and gestational diabetes were all associated with increased risks of maternal hypertension.19 In addition, smoking before and during pregnancy was associated with significantly increased risk of chronic hypertension.19
Data on women of reproductive age (18-49 years) from the 2010-2014 US National Health Interview Survey indicate markedly higher prevalence of CVD, hypertension, diabetes, kidney disease, asthma, and serious psychological distress among non-Hispanic Black and AIAN women, women at older ages, those at lower education and income levels, unmarried (divorced/separated/never married) women, US-born women, current smokers, and women with obesity.18,19 Ethnic-minority and socially-disadvantaged groups in the US differ greatly from the majority, affluent groups in their social, physical, and living environments that might influence pre-existing chronic and medical conditions and related risks such as pre-pregnancy obesity, smoking, gestational diabetes, pregnancy-related hypertension, and weight gain during pregnancy.19 They have limited access to neighborhood amenities such as sidewalks, parks/playgrounds, green spaces, public transportation, and heathy, affordable foods that promote physical activity, healthy lifestyle, and healthy living.19,21 Many of the risk factors identified above are modifiable, and maternal deaths from most of the indirect causes are largely preventable. Several community-based federal programs have been successful in reducing rates of obesity, physical inactivity, smoking, and chronic hypertension and promoting healthy eating and weight management.19-21
4.1. Limitations
This study has limitations. Underreporting of mortality statistics for Hispanics, APIs, and AIANs on the death certificate may lead to an underestimation of maternal mortality rates for these racial/ethnic groups.1,10 Inconsistencies in the reporting of race/ethnicity, educational attainment, marital status, nativity status, and maternal age in numerator (deaths) and denominator (births) databases may lead to misestimation of maternal mortality rates.1,10,11 Because of the small numbers of deaths, our analysis does not show the full extent of racial/ethnic disparities in maternal mortality from indirect causes as overall maternal mortality rates among API and Hispanic subgroups have been shown to vary greatly, with Filipinos and Puerto Ricans, for example, at substantially higher risks of maternal mortality than Chinese, Asian Indians, and Central/South Americans.16
Another limitation refers to the fact that data used in this study come from two different unlinked data sources: national mortality and national natality databases. The natality database was only used to derive the total number of births overall and by social determinants, which were used as denominators to compute maternal mortality rates. This differs from the CDC’s Pregnancy Mortality Surveillance System that links pregnancy-related deaths up to one year to corresponding cohorts of live births and fetal deaths, which allows one to analyze severe maternal morbidity (SMM) outcomes such as hypertensive disorders in pregnancy, eclampsia, obstetric infections, hemorrhage, embolism, uterine rupture, and other pregnancy complications and their impacts on maternal mortality.8,9 Because of the unlinked nature of our data sources, we were unable to carry out detailed individual-level analyses of maternal mortality that are typical of SMM studies. Lastly, the differential adoption of a pregnancy checkbox item on the death certificate by many states may have been a factor influencing the recent trend (or apparent increase or misclassification) in maternal deaths and mortality from indirect causes.1,9,10,16,22,23
5. Conclusions and Global Health Implications
While US maternal mortality from direct obstetric causes has declined during the past two decades, maternal deaths due to indirect causes, particularly from pre-existing medical conditions, including CVD, have increased.1,9,10,16 As is the case with overall maternal mortality16, socially and economically-disadvantaged demographic groups and communities experience 2-to-6 times higher risk of maternal mortality from indirect causes. There is a growing understanding that the contribution of indirect causes is misclassified and underestimated.5,17 Pre-pregnancy obesity, for example, increases the risk of both direct and indirect causes of maternal mortality, including chronic and gestational diabetes, pregnancy-related hypertension, pre-eclampsia and eclampsia, spontaneous abortion, hemorrhage, and uterine rupture.17,19 Yet, obesity is only considered an indirect or contributing condition rather than an underlying cause of maternal death.17 Monitoring social inequalities is important in that they represent the impact of underlying social determinants on both indirect and direct causes of maternal mortality.4,24 Understanding the complex interactions among social determinants, indirect causes, and more proximal direct causes of maternal deaths is important to reducing maternal mortality and improving maternal health.5,17
Compliance With Ethical Standards
Conflicts of Interest: None.
Funding/Support: Dr. Hyunjung Lee was supported in part by an appointment to the Research Participation Program at the Health Resources & Services Administration - Office of Health Equity (HRSA-OHE), administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the US Department of Energy and HRSA.
Ethical approval: No IRB approval was required for this study, which is based on the secondary analysis of public-use federal databases.
Disclaimer: The views expressed are the authors’ and not necessarily those of the Health Resources and Services Administration or the US Department of Health and Human Services.
References
- 2019. Mortality Multiple Cause-of-Death Public Use Data File Documentation. Hyattsville, MD: US Department of Health and Human Services; http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm
- Global, regional, and national levels and causes of maternal mortality during 1990-2013:a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947):980-1004.
- [Google Scholar]
- Global causes of maternal death:a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323-e333.
- [Google Scholar]
- Factors underlying the temporal increase in in maternal mortality in the United States. Obstet Gynecol. 2017;129(1):91-100.
- [Google Scholar]
- Trends in maternal mortality by socio-demographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol. 2017;129(5):811-818.
- [Google Scholar]
- Racial/ethnic disparities in pregnancy-related deaths - United States, 2007-2016. MMWR. 2019;68(35):762-765.
- [Google Scholar]
- Pregnancy-related mortality in the United States 1998 to 2005. Obstet Gynecol. 2010;116(6):1302-1309.
- [Google Scholar]
- All-cause and cause-specific mortality among US youth:socioeconomic and rural-urban disparities and international patterns. J Urban Health. 2013;90(3):388-405.
- [Google Scholar]
- Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93(7):1137-1143.
- [Google Scholar]
- Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25-64 years by area socioeconomic status 1969-1998. Int J Epidemiol. 2002;31(3):600-613.
- [Google Scholar]
- Socioeconomic and racial/ethnic disparities in cancer mortality incidence, and survival in the United States 1950-2014:over six decades of changing patterns and widening Inequalities. J Environ Public Health DOI:2017/2819372 Epub March 2017
- [Google Scholar]
- Trends and social inequalities in maternal mortality in the United States, 1969-2018. Int J MCH AIDS. 2021;10(1):11-24.
- [Google Scholar]
- Maternal mortality:direct or indirect has become irrelevant. Lancet Global Health. 2017;5(12):e11813.
- [Google Scholar]
- 2015. The National Health Interview Survey Questionnaires, Datasets and Related Documentation: 2010-2014 Public Use Data Files. Hyattsville, MD: US Department of Health and Human Services; http://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm
- Racial/Ethnic nativity, and sociodemographic disparities in maternal hypertension in the United States, 2014-2015. Int J Hypertens 2018 May 17 DOI:10.1155/2018/7897189
- [Google Scholar]
- Marked disparities in pre-pregnancy obesity and overweight prevalence among US women by race/Ethnicity nativity/immigrant status and sociodemographic characteristics, 2012-2014. J Obes 2019 February DOI:10.1155/2019/2419263
- [Google Scholar]
- Neighborhood Socioeconomic Conditions Built Environments and Childhood Obesity. Health Aff. 2010;29(3):503-512.
- [Google Scholar]
- Evaluation of the pregnancy status checkbox on the identification of maternal deaths. Natl Vital Stat Rep. 2020;69(1):1-25.
- [Google Scholar]
- Maternal mortality in the United States:changes in coding publication, and data release 2018. Natl Vital Stat Rep. 2020;69(2):1-18.
- [Google Scholar]
- Ending preventable maternal mortality:phase II of a multi-step process to develop a monitoring framework, 2016-2030. BMC Pregnancy Childbirth. 2018;18(1):258. https://doi.org/10.1186/s12884-018-1763-8
- [Google Scholar]





